
Why Am I Always Cold Even in Warm Weather?
⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission — at no extra cost to you — if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
Even when the sun is shining or the air conditioner is on full blast, do you find yourself bundled in sweaters while others are sweating in tank tops? If you’re always cold even in warm weather your body might be trying to tell you something important. In this post, we’ll explore the possible medical and nutritional reasons behind persistent cold sensitivity, including when to seek help and what you can do to warm up naturally.
Table of Contents:
- Is It Normal to Always Feel Cold?
- Common Medical Reasons You Might Feel Cold
- Remedies and Warmth Hacks That Help
- When to See a Doctor
- Final Thoughts: Cold Is a Clue, Not Just a Quirk
Is It Normal to Always Feel Cold?
Feeling cold from time to time is completely normal, you might have just walked out of an air-conditioned room, skipped a meal, or spent hours sitting still. In these situations, your body is responding appropriately to temporary changes in environment or energy availability.
The concern begins when cold sensitivity becomes persistent. If you regularly feel cold while others around you are comfortable, your body may be signaling that something deeper is going on. Your ability to stay warm depends on thermoregulation, the system that keeps your internal temperature stable. This process is controlled by the brain, especially the hypothalamus, and supported by thyroid hormones, healthy circulation, adequate muscle mass, sufficient body fat, and proper nutrient availability. When one or more of these components is impaired, heat production or heat distribution suffers, leading to ongoing coldness.
Before assuming a medical cause, it is important to rule out common non-medical factors that can make anyone feel cold:
Recent exposure to strong air conditioning
Wet or damp clothing
Being significantly underweight
Skipping meals, fasting, or low calorie intake
Poor sleep or prolonged inactivity
Mental health conditions such as anxiety or depression, which can alter nervous system responses
If these factors do not apply and the sensation of cold keeps returning, especially in warm environments, it is unlikely to be random. Recurrent cold intolerance is often the body’s early warning sign that metabolism, circulation, hormones, or nutrition may be out of balance.
At that point, it is worth looking beyond surface explanations and exploring the medical reasons that commonly drive persistent cold sensitivity.
Common Medical Reasons You Might Feel Cold
1. Anemia:
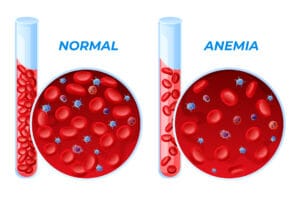
Anemia develops when your body does not have enough healthy red blood cells or sufficient hemoglobin to carry oxygen to tissues. Iron deficiency is the most common cause, but anemia can also result from chronic inflammation, vitamin B12 or folate deficiency, kidney disease, or ongoing blood loss such as heavy menstrual bleeding.
When oxygen delivery drops, your body prioritizes vital organs like the heart, brain, and kidneys. Blood flow to the skin and extremities is reduced, which is why people with anemia often experience cold hands and feet even in warm environments.
Common symptoms include:
Persistent chills or cold intolerance
Fatigue and weakness
Pale skin
Headaches or lightheadedness
Shortness of breath with minimal exertion
A simple blood test checking hemoglobin and iron stores can confirm anemia. If levels are low, focus on iron-rich foods such as red meat, liver, beans, lentils, spinach, and fortified grains. Iron supplements should only be started after testing and under medical guidance to avoid side effects or iron overload.
2. Hypothyroidism:
Your thyroid gland, located at the front of your neck, produces hormones that regulate metabolism and heat production. When the thyroid underperforms, a condition known as hypothyroidism, metabolic processes slow down across the body because heat generation is tied directly to metabolism, people with hypothyroidism often feel cold even in hot weather.
Additional symptoms may include:
Weight gain
Fatigue and sluggishness
Constipation
Hair thinning or hair loss
Depression or brain fog
Tests to consider:
Thyroid Stimulating Hormone (TSH), Free T4, and Free T3 blood tests help assess thyroid function accurately.
3. Poor Circulation:
Adequate circulation is essential for distributing warm blood throughout the body. When blood flow is impaired, heat cannot reach the hands, feet, ears, or nose efficiently.
Signs of poor circulation include:
Ice-cold fingers or toes
Numbness or tingling
Color changes in the skin
Common causes include:
Smoking
Sedentary lifestyle
Diabetes
Cardiovascular disease
Blood clots
Tight clothing or compression garments
Regular movement, avoiding smoking, loosening tight socks or wristbands, and elevating your legs occasionally can improve circulation and reduce cold sensitivity.
4. Low Body Fat:
Body fat acts as insulation, helping the body retain heat. Individuals with very low body fat often struggle to stay warm, even when their health is otherwise good.
This is commonly seen in underweight individuals, endurance athletes, dancers, or people with restrictive eating patterns or eating disorders.If this applies to you, it is important not to dismiss the symptom. Supporting adequate nutrition and energy intake is key. In the meantime, practical measures such as electric blankets, heated pads, thermal socks, and layered clothing can help maintain comfort.
5. Raynaud’s Disease:
Raynaud’s phenomenon causes an exaggerated narrowing of blood vessels in response to cold exposure or emotional stress. This sudden reduction in blood flow typically affects the fingers and toes.
Typical color changes occur in stages:
White from reduced blood flow
Blue from low oxygen levels
Red when circulation returns
People at higher risk include:
Women under 40
Individuals with autoimmune diseases
Smokers
People exposed to repetitive vibration from tools or equipment
Management strategies include:
Wearing gloves, avoiding caffeine and nicotine, managing stress, using hand warmers, and discussing medication options such as calcium channel blockers with a doctor if symptoms are severe.
6. Medications That Affect Body Temperature:
Several commonly prescribed medications can interfere with heat regulation without people realizing it.
- Beta-blockers
Used to treat high blood pressure and heart conditions, these medications slow heart rate and may reduce blood flow to the extremities, leading to cold hands and feet. - Sedatives and sleep aids
These suppress nervous system activity and lower metabolic rate, reducing heat production, especially at night. - Antidepressants
Certain SSRIs and SNRIs can alter serotonin pathways involved in temperature regulation, contributing to cold intolerance in some individuals. - Diuretics
Often called water pills, medications like furosemide can deplete electrolytes such as magnesium and potassium, which play a role in muscle function and thermoregulation.
Any medication-related cold sensitivity should be discussed with a healthcare provider before making changes.
7. Nutritional Deficiencies That Affect Heat Production:
Even mild nutrient deficiencies can interfere with your body’s ability to generate and distribute heat efficiently.
- Iron deficiency
Covered above under anemia. - Vitamin B12
Essential for red blood cell formation and nerve health. Deficiency can cause cold hands and feet, tingling sensations, fatigue, and memory problems. Vegans and older adults are at higher risk and may need fortified foods or supplementation. - Magnesium
Supports muscle contraction, nerve signaling, and circulation. Low magnesium levels can worsen cold sensitivity.
Good dietary sources include nuts, seeds, whole grains, legumes, and leafy green vegetables.
8. Hormonal Imbalances: A Common Hidden Driver:
Hormones play a central role in temperature regulation and energy balance.
- Estrogen and progesterone
Fluctuations during the menstrual cycle, perimenopause, or menopause can disrupt signals in the hypothalamus, the brain’s temperature control center. This may cause chills, alternating hot flashes, sweating, or cold intolerance. - Cortisol
Chronic stress can dysregulate cortisol production, leading to fatigue, immune suppression, and increased sensitivity to cold.
Signs that hormones may be involved include:
Mood swings
Irregular or missed periods
Hair thinning
Sudden cold spells
Difficulty sleeping
When cold sensitivity is persistent and unexplained, evaluating hormonal health is often an essential part of finding the root cause.
Home Remedies and Warmth Hacks That Help
Whether it’s hormonal, nutritional, or circulatory, these natural hacks can help:
- layer up smartly, thin layers trap heat better than bulky coats.
- Warm drinks, herbal teas, turmeric lattes, or hot broths help boost internal warmth. Also read-Bedtime Herbal Tea for Anxious Sleep and Cortisol Reduction.
- Eat heat-producing foods like ginger, garlic, oats, chili pepper, and protein-rich meals.
- Stay active: Move every hour, it improves blood flow.
- Use heating tools, heated gloves,rechargeable hand warmers, thermal socks,electric vests.
- Hydrate: Even mild dehydration can worsen cold sensitivity.
When to See a Doctor
Feeling cold once in a while is rarely a problem. However, persistent or worsening cold intolerance should not be ignored, especially when it appears without an obvious trigger. In some cases, it can be an early sign of an underlying medical condition that requires evaluation and treatment.
You should contact a healthcare professional if feeling cold is ongoing and accompanied by any of the following symptoms:
Unexplained weight loss or weight gain
Dizziness, lightheadedness, or fainting spells
Pale, bluish, or numb fingers and toes
Changes in your menstrual cycle or fertility
Hair thinning, hair loss, or brittle nails
Severe or persistent fatigue that interferes with daily life
A personal or family history of autoimmune disease
These warning signs suggest that the issue may involve your blood, thyroid, hormones, circulation, or immune system rather than simple environmental exposure.
What Tests to Ask For:
Blood work is often the most effective first step in identifying the cause of cold sensitivity. Useful tests may include:
Complete Blood Count (CBC) to evaluate for anemia or infection
Thyroid panel including TSH, Free T4, and Free T3 to assess metabolic function
Vitamin and mineral levels, especially iron, vitamin B12, vitamin D, and magnesium
Hormone testing, particularly for women experiencing menstrual irregularities, perimenopause, or unexplained fatigue
Early testing helps catch issues before they progress and allows treatment to be targeted rather than guesswork. If cold intolerance is affecting your quality of life, seeking medical input is not overreacting. It is a practical step toward understanding what your body is trying to communicate.
Final Thoughts: Cold Is a Clue, Not Just a Quirk
Feeling cold all the time is not something to normalize or ignore. When your body keeps sending the same signal, it usually means something is out of balance. Temperature sensitivity is one of the quieter ways your system asks for attention.
Rather than focusing only on staying warm, the goal should be understanding why the cold is happening. Issues with nutrition, thyroid function, circulation, hormones, or medication effects often show up this way long before more serious symptoms appear.
A clear, step by step approach makes a difference:
Eliminate obvious environmental and lifestyle causes
Evaluate body weight, diet quality, and meal timing
Check thyroid health and overall energy levels
Run basic blood tests to uncover anemia or deficiencies
Review medications that may affect circulation or metabolism
Addressing the root cause is far more effective than layering clothes or turning up the heat. When you listen early and act deliberately, cold intolerance becomes a useful clue rather than a lingering problem, your body is not being difficult it is being informative.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowSuggested Post:
- What Your Tongue Can Reveal About Vitamin Deficiencies
- Iron Supplement Side Effects: What You Need to Know Before You Start.
- 13 Sneaky Signs of Magnesium Deficiency in Women (And How to Fix It Naturally)
- 12 Powerful insights Into What Your Diet Really Needs (micronutrients and Supplements)
- Correct Iron Deficiency with Food Fast: Expert Timeline + 7-Day Meal Plan
- 7 Critical Facts You Must Know: How to Choose the Right Multivitamin
- 15 Powerful Home Remedies for Constipation That Really Work
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


