⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission — at no extra cost to you — if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
7 Powerful Insights on Osteoporosis in Women Under 50
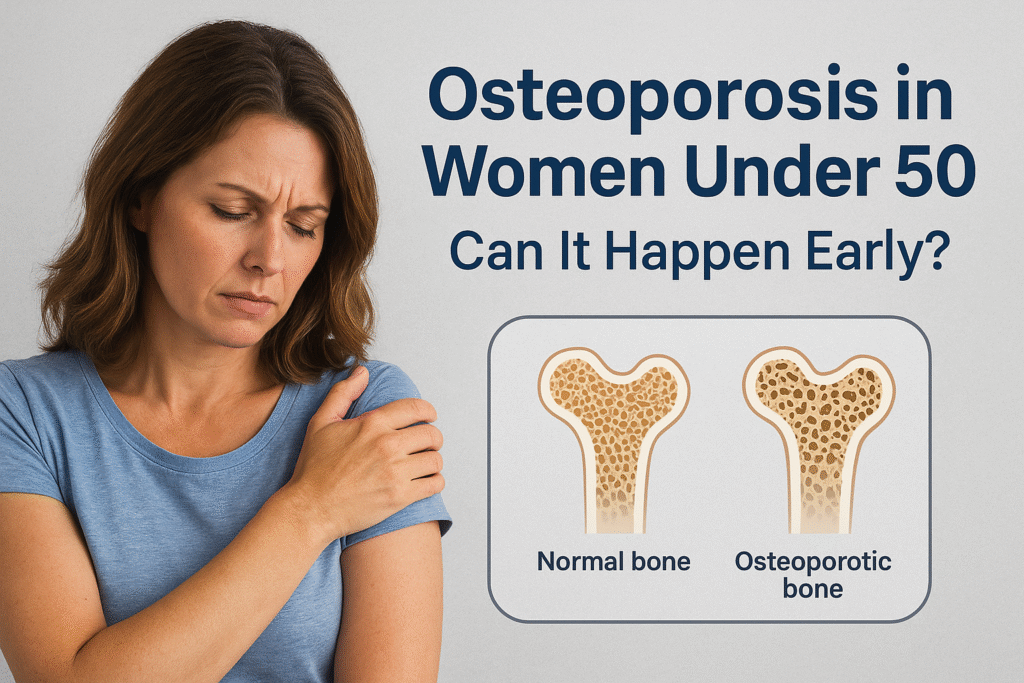
Osteoporosis in Women Under 50: Can It Happen Early?
When most people think of osteoporosis, they imagine an older, postmenopausal woman being advised to take calcium supplements or avoid falls. While it is true that osteoporosis is far more common after menopause, the condition is not limited to older age. Women under 50 can, and sometimes do, develop osteoporosis, often without realizing it until a fracture occurs.
The question then arises, why would younger women, who are generally considered to be in their peak bone years, experience bone fragility? The answer is rarely straightforward. In women under 50, osteoporosis almost always points to an underlying factor, whether hormonal, genetic, medical, or lifestyle-related that accelerates bone loss or disrupts bone formation.
Early-onset osteoporosis matters because the consequences extend far beyond a broken bone. Fragile bones at a young age can mean decades of higher fracture risk, potential limitations on physical activity, and long-term effects on overall health. The earlier it develops, the greater the lifetime impact.
In this article, we’ll explore:
- What osteoporosis is and how it affects the body
- Why it can occur in women under 50
- The key symptoms and red flags to look out for
- How it’s diagnosed in younger women
- Strategies to protect and strengthen bone health before menopause
By the end, you’ll understand not only how osteoporosis can happen early but also what steps younger women can take to reduce risk and safeguard their bones for the future.
What Is Osteoporosis?
Osteoporosis is a condition where bones gradually lose their density and structural strength, making them fragile and prone to fractures. Although bones may seem solid and unchanging, they are actually living tissue that is constantly renewed through a process called remodeling.
- Bone breakdown (resorption): Old bone is broken down by specialized cells called osteoclasts.
- Bone rebuilding (formation): New bone is laid down by osteoblasts to replace what was lost.
In a healthy adult, these two processes remain in balance, keeping bones strong and resilient. In osteoporosis, however, bone breakdown occurs faster than bone rebuilding. Over time, this imbalance leaves bones porous and brittle.
- Normal bone: Dense with tightly packed structures and small spaces.
- Osteoporotic bone: Fragile with larger holes and weakened support, much like a sponge.
Because of this reduced strength, even minor stress or falls can result in fractures. The most vulnerable areas include the spine, hips, and wrists, fractures here often cause the greatest disability and long-term complications.
Can Osteoporosis Really Affect Women Under 50?
Yes. Although osteoporosis is more common after menopause, it can also occur in younger women, including those under 50. Research suggests that about 1-2% of premenopausal women may have bone density low enough to qualify as osteoporosis.
The critical difference is that in younger women, osteoporosis almost always points to an underlying factor beyond natural aging, these may include:
- Hormonal imbalances, such as low estrogen from early menopause or irregular periods.
- Chronic illnesses, like autoimmune or gastrointestinal diseases, that interfere with nutrient absorption or bone metabolism.
- Long-term medication use, especially corticosteroids or certain cancer treatments.
- Lifestyle factors such as smoking, malnutrition, or lack of weight-bearing activity.
Because bone loss at a younger age is unusual, identifying and addressing these secondary causes is essential. Unlike age-related bone thinning, many of these factors are treatable — and in some cases, reversing the cause can restore bone strength and reduce long-term fracture risk.
Causes of Osteoporosis in Younger Women
Osteoporosis in women under 50 is rarely due to aging alone. Instead, it usually signals secondary factors that accelerate bone loss or disrupt bone formation. The most common causes fall into five categories:
1. Hormonal Factors
Estrogen plays a central role in maintaining bone density. When estrogen levels drop significantly, bone breakdown speeds up.
- Early menopause or premature ovarian insufficiency (POI): Women who lose ovarian function before age 40 face rapid bone loss because of reduced estrogen.
- Amenorrhea (absence of periods): Often seen in athletes, dancers, or women with eating disorders, this condition lowers estrogen production and compromises bone health.
- Polycystic ovary syndrome (PCOS): Some women with PCOS experience irregular ovulation and hormonal imbalances that may indirectly affect bone metabolism.
2. Medical Conditions
Chronic illnesses can interfere with bone strength either directly or through treatments.
- Autoimmune diseases: Conditions such as rheumatoid arthritis, lupus, and inflammatory bowel disease increase bone loss due to inflammation and frequent corticosteroid use.
- Celiac disease: Poor absorption of calcium and vitamin D can silently weaken bones if the condition goes undiagnosed.
- Endocrine disorders: Hyperthyroidism, hyperparathyroidism, and uncontrolled diabetes all accelerate bone turnover.
- Kidney and liver disease: Both organs play roles in vitamin D activation and mineral balance, so dysfunction can impair bone strength.
3. Medications
Several long-term medications are known to negatively affect bone density:
- Corticosteroids (e.g., prednisone): Among the most common culprits, especially with prolonged use.
- Anti-seizure medications: Some alter vitamin D metabolism and calcium balance.
- Cancer therapies: Chemotherapy and aromatase inhibitors reduce estrogen or damage bone-forming cells.
- Proton pump inhibitors (PPIs): Widely used for acid reflux, these may reduce calcium absorption when used over many years.
4. Lifestyle Risk Factors
Daily habits strongly influence bone health. Risk factors include:
- Low body weight: Associated with lower estrogen levels and reduced bone reserves.
- Nutrient-poor diet: Insufficient calcium, vitamin D, and protein all compromise bone structure.
- Smoking: Directly damages bone-forming cells and lowers estrogen.
- Excessive alcohol: Disrupts calcium absorption and bone repair.
- Physical inactivity: Lack of weight-bearing or strength-building activity weakens bones over time.
5. Genetic Predisposition
Family history plays a powerful role. Women whose mothers or grandmothers had osteoporosis or frequent fractures are at greater risk, even if they live healthy lifestyles.
Symptoms of Osteoporosis in Younger Women
Osteoporosis is often called the “silent disease” because it develops without obvious symptoms. Many women only discover they have it after a fracture. Still, there are some warning signs that may appear in younger women:
- Stress fractures: Small fractures that occur from minor falls or even regular physical activity.
- Loss of height: Gradual shrinking may indicate vertebral fractures in the spine.
- Persistent back pain: Sometimes caused by compression fractures in spinal bones.
- Stooped posture (kyphosis): Forward rounding of the upper back due to weakened spinal bones.
Because these signs often appear late, early screening is critical for women at risk.
Risk Factors Unique to Younger Women
While osteoporosis in younger women is uncommon, certain risk factors are particularly relevant in this age group and can accelerate bone loss.
Female Athlete Triad / RED-S (Relative Energy Deficiency in Sport):
Women who engage in high-intensity training without adequate calorie intake may experience irregular or absent periods, low estrogen, and reduced bone density. Stress fractures are often the first sign of this imbalance.
Eating Disorders:
Conditions such as anorexia and bulimia severely limit nutrient intake, especially calcium and vitamin D, while also lowering body weight and estrogen levels. Together, these factors significantly weaken bones.
Extreme Dieting and Restrictive Eating Patterns:
Popular diet trends, such as prolonged fasting, carb elimination, or dairy avoidance without alternatives, can deprive bones of essential nutrients.
- Chronic Stress: High cortisol levels from unmanaged stress can impair bone building, mimicking some of the effects of steroid medication.
These unique factors mean that younger women should not dismiss irregular periods, fatigue, or frequent stress injuries as “normal.” They may be early warning signs of compromised bone health.
Fractures in Younger Women: A Hidden Clue
One of the earliest signs of osteoporosis in premenopausal women is often a fracture that seems “out of proportion” to the cause.
- Stress fractures: Small cracks in the bone that occur during normal activities like running or walking.
- Low-impact fractures: Breaks that happen after a minor fall, such as tripping on a step or slipping on a flat surface.
- Recurrent fractures: Multiple fractures over a short period, especially in the feet, hips, or spine.
Because younger women are expected to have strong bones, these injuries are sometimes dismissed as accidents or sports injuries. However, repeated or unusual fractures should always prompt a deeper evaluation for osteoporosis or other bone-weakening conditions.
How The Role of Pregnancy and Postpartum in Bone Health
Pregnancy and breastfeeding place unique demands on a woman’s bones. During these times, the body prioritizes providing calcium to the growing baby and to breast milk, sometimes at the expense of the mother’s bone density.
Pregnancy-associated osteoporosis (PAO):
A rare but recognized condition in which women develop osteoporosis during late pregnancy or shortly after delivery, often leading to vertebral fractures.
Breastfeeding and calcium:
Prolonged breastfeeding without sufficient calcium and vitamin D intake can temporarily lower bone density, though most women recover after weaning.
Multiple pregnancies:
Repeated pregnancies without proper nutritional support can increase long-term bone health risks.
The good news is that in most cases, bone density lost during pregnancy and breastfeeding is partially or fully restored once normal menstrual cycles return and nutrition is adequate. Still, these phases of life highlight how important it is for younger women to enter pregnancy with strong bones and to maintain proper nutrition throughout.
Is Osteoporosis Diagnosed in Women Under 50?
Diagnosing osteoporosis in younger women requires a careful and thorough approach. Because bone loss before menopause is unusual, doctors look not only at bone density but also at the possible underlying causes.
1. Bone Density Test (DEXA Scan)
The dual-energy X-ray absorptiometry (DEXA) scan is the gold standard for measuring bone mineral density (BMD).
- T-score: Compares a woman’s bone density to that of a healthy 30-year-old. This is commonly used in postmenopausal women.
- Z-score: Compares bone density to other women of the same age, sex, and body size. For women under 50, the Z-score is more meaningful, since a low Z-score suggests something abnormal for that age group.
A Z-score of –2.0 or lower typically indicates unusually low bone density and prompts further investigation.
2. Blood Tests
Bloodwork can reveal underlying medical problems that may be contributing to bone loss. Tests often include:
- Calcium and vitamin D levels
- Thyroid function tests
- Parathyroid hormone levels
- Markers of inflammation or autoimmune disease
- Reproductive hormones (estrogen, FSH, LH)
3. Medical History and Lifestyle Assessment
A detailed health history provides essential context. Doctors usually review:
- Menstrual and reproductive history (including early menopause or irregular cycles).
- Past fractures or injuries.
- Medication use (especially steroids or cancer therapies).
- Family history of osteoporosis or fractures.
- Diet, exercise patterns, smoking, and alcohol intake.
This comprehensive assessment ensures that osteoporosis in a younger woman is not mistaken for age-related thinning, but rather evaluated in light of potential secondary causes.
Why Early-Onset Osteoporosis Matters
Osteoporosis before the age of 50 is more than a short-term health issue, it carries long-lasting consequences that can shape a woman’s future well-being.
- Higher lifetime fracture risk: Weak bones at a young age mean decades of exposure to fracture risk, with injuries often occurring from minor falls or everyday activities.
- Reduced quality of life: Recurrent fractures can lead to chronic pain, physical limitations, and even loss of independence.
- Pregnancy and fertility considerations: Bone health may influence pregnancy outcomes, particularly if calcium demands increase during gestation and breastfeeding.
- Psychological impact: Living with osteoporosis in early adulthood or midlife can affect mental health, leading to anxiety about fractures, body image concerns, or reduced confidence in physical activity.
In short, early-onset osteoporosis is not simply a medical condition, it can reshape how a woman lives, works, and plans for her future. Recognizing it early allows for proactive management that can significantly reduce long-term risks.
Prevention and Lifestyle Strategies
For women under 50, prevention is the most powerful tool against osteoporosis. Building and maintaining strong bones during these years creates a protective “bone bank” for later life. Lifestyle choices play a central role in supporting bone density.
1. Nutrition for Strong Bones
Good nutrition is the foundation of bone health.
- Calcium: Aim for 1,000-1,200 mg per day through a combination of food and supplements if necessary. Sources include dairy products, fortified plant-based milk, tofu, sardines, almonds, and leafy greens.
- Vitamin D: Essential for calcium absorption. The body produces it through sunlight exposure, but dietary sources like fatty fish, eggs, and fortified foods can help. Supplements are often recommended, especially in regions with limited sun.
- Protein: Adequate protein supports the bone matrix, the structural framework that holds minerals in place. Both animal and plant proteins are beneficial.
- Other micronutrients: Magnesium, zinc, and vitamin K2 all contribute to bone strength and proper calcium utilization.
2. Exercise and Movement
Bones grow stronger when they are challenged by movement and weight.
- Weight-bearing exercises: Walking, jogging, stair climbing, and dancing stimulate bone-building activity.
- Strength training: Lifting weights or using resistance bands improves bone density while building muscle to support and protect bones.
- Balance and flexibility training: Yoga, Pilates, and tai chi improve coordination and reduce the risk of falls, a crucial factor in preventing fractures.
3. Lifestyle Habits
Small but consistent lifestyle choices have a large impact on bone health.
- Quit smoking: Smoking damages bone cells, reduces estrogen levels, and speeds up bone loss.
- Limit alcohol: Excessive drinking disrupts calcium absorption and interferes with bone remodeling.
- Avoid extreme dieting: Very low-calorie or restrictive diets can reduce both nutrient intake and hormone levels, undermining bone health.
Medical Treatment Options for Younger Women
When osteoporosis develops before age 50, treatment must be carefully tailored. Unlike postmenopausal osteoporosis, the focus is not only on strengthening bone but also on correcting the root cause.
- Hormone therapy: Women with early menopause or estrogen deficiency may benefit from hormone replacement, which can slow bone loss and restore balance.
- Bisphosphonates: Commonly prescribed in older women, these drugs reduce bone breakdown. However, their long-term safety in premenopausal women is less established, so they are used cautiously.
- Denosumab or teriparatide: Advanced therapies that may be considered in severe cases, particularly when fractures occur or bone density is extremely low.
- Correcting underlying conditions: Treating celiac disease, adjusting thyroid medication, reducing long-term steroid use, or addressing malnutrition can significantly improve bone health without the need for lifelong medication.
In younger women, treatment is rarely “one-size-fits-all.” Instead, doctors aim to address the underlying trigger of bone loss while providing supportive strategies to restore strength and reduce future risk.
Key Takeaways
- Osteoporosis is not just an “older woman’s disease.” Women under 50 can develop it, though it is less common.
- Secondary causes are usually responsible. Hormonal changes, chronic illnesses, long-term medications, and lifestyle factors often play a role.
- Symptoms are often silent. Many women don’t realize they have osteoporosis until a fracture occurs.
- Accurate diagnosis is essential. A bone density scan (DEXA) combined with blood tests and lifestyle assessment helps identify the cause.
- Prevention is possible. Strong nutrition, weight-bearing exercise, and healthy lifestyle choices build and protect bone density.
- Treatment should be personalized. Younger women require tailored care that addresses both bone health and the underlying condition driving bone loss.
Conclusion
Osteoporosis in women under 50 may be rare, but when it happens, it is far from trivial. Early-onset bone loss often signals deeper health concerns such as hormonal imbalance, autoimmune disease, nutritional deficiencies, or the effects of medication. Left unaddressed, it can set the stage for a lifetime of fractures, chronic pain, and reduced independence.
The encouraging news is that osteoporosis in younger women is not a dead end, with early detection, targeted treatment, and proactive lifestyle strategies, it is possible to slow, stop, or even reverse bone loss. Every step — from eating a nutrient-rich diet to staying physically active and addressing medical conditions helps protect your bones.
If you are under 50 and notice risk factors such as irregular periods, frequent fractures, family history of osteoporosis, or autoimmune disease, speak to your healthcare provider. A timely bone health assessment could make the difference between fragile bones and lifelong strength.
Because ultimately, strong bones aren’t just about aging gracefully, they’re about living fully, confidently, and without limits at every stage of life.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Blog Post You Might Like:
- 10 Shocking Heart Attack Symptoms in Women That Look Nothing Like Men’s
- 10 Powerful Facts About Hormonal Contraceptives You Must Know
- 10 Powerful Facts About Hormonal Contraceptives You Must Know
- Mid-Cycle Spotting Explained: 10 Key Facts About Ovulation Bleeding
- How Long Before Estrogen Cream Works: 3 Proven Timelines for Vaginal Dryness Relief
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


