⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission — at no extra cost to you — if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
15 Shocking Ways Low-Grade Inflammation Is Sabotaging Your Health
Most people imagine inflammation as something obvious, swelling, redness, heat, or pain. Those reactions are easy to spot because they’re part of your body’s emergency defense system. You sprain an ankle, catch an infection, or cut your skin, and your immune system rushes in with a powerful surge of inflammation designed to protect and heal, but there’s a more dangerous version that almost no one notices until it’s too late.
A form of inflammation that doesn’t scream, it whispers.
It doesn’t make you limp or wince. It operates quietly in the background, slowly wearing down your internal systems day after day.
This silent biological pressure is called chronic low-grade inflammation and it’s one of the most overlooked drivers of aging, disease, and physical decline. You won’t feel it the way you feel a sprain or fever, but you will feel its consequences over the years, slower metabolism, reduced energy, hormonal imbalance, joint stiffness, brain fog, weight changes, and a gradual loss of resilience.
It is so persistent and destructive that researchers now refer to it as inflammaging, the type of aging that isn’t caused by time, but by constant immune irritation.
It doesn’t strike suddenly,
it builds slowly, it shapes how rapidly you age, how well your organs function, how vibrant or drained you feel, and how long you remain truly healthy.
This article breaks down what low-grade inflammation really does inside your body as you grow older and why learning to control it may be one of the most powerful decisions you make for your long-term health, longevity, and quality of life.
What Is Low-Grade Inflammation?
Low-grade inflammation is a quiet, persistent activation of your immune system that continues even when there is no injury, infection, or immediate threat to respond to. Unlike acute inflammation, which is sharp, intense, and essential for healing, this form is slow, subtle, and ongoing. You don’t feel heat, swelling, or pain, but the underlying biological activity never really stops.
Instead of turning on and off the way a normal immune response should, low-grade inflammation operates like a dimmer switch stuck halfway. It is always active, always signaling, always creating small amounts of cellular stress.
It is:
- slow-burning rather than intense
- continuous or frequently recurring
- internally focused and not visible on the surface
- easy to overlook because it doesn’t produce dramatic symptoms
- driven by lifestyle habits, environmental exposures, and metabolic changes
The best way to visualize it is to imagine a tiny flame inside a house. It doesn’t engulf the rooms or collapse the walls in a single day. But if that flame is allowed to smolder for years, it weakens beams, corrodes wiring, and slowly compromises the entire structure. Low-grade inflammation works the same way, quiet, persistent, and cumulatively destructive.
Why Low-Grade Inflammation Increases With Age
Although aging itself naturally shifts the immune system, the modern lifestyle accelerates inflammation far beyond what biology intended. As the years pass, multiple internal systems become more vulnerable and less efficient, creating a perfect environment for chronic inflammation to thrive.
Below are the key reasons it becomes more common with age:
1. Immune System Wear-and-Tear
The immune system is designed to be precise and targeted. Over time, however, repeated exposure to infections, stress, toxins, poor diet, and environmental irritants gradually erodes its accuracy. Instead of responding only when necessary, it begins firing off low-level inflammatory signals even in the absence of threats. This constant background noise is one of the early hallmarks of inflammaging.
2. Accumulated Cellular Damage
Every cell in your body experiences wear from daily life, oxidative stress, environmental pollutants, metabolic byproducts, and nutrient deficiencies. When cells become damaged, they release distress molecules that activate the immune system. A younger body clears this damage efficiently. An older body does not, the result is a steady trickle of inflammatory signaling that never fully shuts off.
3. Visceral Fat
Fat stored deep around the abdominal organs is biologically active. It produces inflammatory hormones and immune chemicals that circulate through the bloodstream, with age, people tend to store more fat in this area, even if their overall weight doesn’t change dramatically. This visceral fat acts like an internal inflammation factory, constantly stimulating the immune response.
4. Poor Gut Integrity
The lining of the digestive tract acts as a barrier between the bloodstream and the outside world. Aging, stress, antibiotics, alcohol, and processed foods can weaken this barrier. When the gut becomes more permeable, small particles that should remain inside the intestines slip into the bloodstream. The immune system detects these particles as threats and responds with chronic inflammation. This mechanism is a major contributor to inflammatory aging.
5. Hormonal Changes
Hormones like estrogen, testosterone, progesterone, melatonin, growth hormone, and DHEA play direct roles in calming the immune system. As these hormones decline with age, the natural checks and balances that prevent inflammation weaken. This hormonal shift alone can raise inflammatory levels even in otherwise healthy people.
6. Mitochondrial Decline
Mitochondria produce energy for your cells. As you age, mitochondrial function deteriorates. When mitochondria weaken, they produce more oxidative stress and fewer clean energy molecules. This creates cellular debris and inflammatory byproducts that irritate the immune system. Mitochondrial dysfunction is considered one of the core biochemical drivers of accelerated aging.
7. Chronic Stress
Long-term stress disrupts cortisol, the hormone responsible for regulating inflammation. When cortisol is chronically high, chronically low, or fluctuates excessively, the immune system becomes dysregulated. Instead of responding appropriately, it overreacts and maintains inflammation even when no danger exists.
All these changes combine to create a biological environment where inflammation is no longer a temporary reaction but a constant presence. What should be an occasional protective response becomes a default operating mode. And because this process is subtle and slow, many people don’t realize it’s happening until symptoms or chronic conditions appear later in life.
How Low-Grade Inflammation Affects Your Health as You Age
Chronic low-grade inflammation is tied to nearly every major chronic disease but beyond the medical diagnoses, it quietly drives the day-to-day symptoms people assume are simply part of getting older. In reality, many of these changes are not from age itself, they are the result of years of silent immune activation.
Below is a deeper look at how this type of inflammation affects every major system in the body.
1. It Accelerates Biological Aging
Your chronological age reflects how long you’ve been alive. Your biological age reflects how well your body is functioning on a cellular level. Low-grade inflammation accelerates the processes that determine biological age, including:
- shortening of telomeres
- impaired cellular repair and turnover
- mitochondrial decline
- accumulation of damaged proteins
- increased DNA replication errors
People with elevated inflammatory markers consistently show signs of being biologically older, even when they share the same chronological age as someone with low levels of inflammation. The outcome is straightforward: inflammation makes you age faster than time alone ever could.
2. It Raises Your Risk of Heart Disease
Inflammation is deeply involved in cardiovascular decline. It disrupts the heart and blood vessels at nearly every stage:
- it injures and irritates blood vessel walls
- it oxidizes LDL cholesterol, making it more dangerous
- it accelerates plaque buildup inside arteries
- it destabilizes existing plaque, increasing the risk of rupture
- it stiffens arteries, contributing to high blood pressure
This explains why individuals with high C-reactive protein (CRP) levels face increased risks of hypertension, heart attacks, strokes, and coronary artery disease, even if their cholesterol is normal. Inflammation is often the hidden factor pushing cardiovascular disease forward.
3. It Promotes Weight Gain and Makes Fat Loss Harder
Inflammation alters the hormonal and metabolic systems that regulate hunger, fat storage, and energy production. It:
- reduces insulin sensitivity
- raises blood sugar
- increases cortisol
- disrupts thyroid hormone conversion
- reduces leptin sensitivity
- slows metabolic rate
These effects make stubborn belly fat, prediabetes, metabolic syndrome, and insulin resistance far more likely. Even with a healthy diet and exercise, inflammation can keep the body in a state where fat loss becomes an uphill battle.
4. It Damages the Brain and Accelerates Cognitive Decline
Low-grade inflammation affects the brain more than most people realize. Inflammatory molecules can cross the blood-brain barrier and activate microglia, the brain’s immune cells. When microglia stay switched on for too long, they begin harming neurons.
This contributes to:
- memory loss
- decreased focus
- slower mental processing
- mood instability
- sleep disturbances
- a higher risk of Alzheimer’s
- increased rates of depression and anxiety
Researchers now consider chronic inflammation to be a core factor in neurodegenerative disorders.
5. It Weakens the Immune System
Low-grade inflammation places constant pressure on the immune system. Instead of working efficiently, the immune response becomes dysregulated. The result is the paradox of being both overactive and ineffective at the same time.
This leads to:
- frequent colds or infections
- slower wound healing
- longer recovery after illness
- higher susceptibility to viruses
- reactivation of dormant infections, such as shingles
As you age, this imbalance contributes to increased fragility and reduced resilience.
6. It Damages Joints and Connective Tissue
You don’t need a formal arthritis diagnosis to feel the effects of chronic inflammation on your joints. Low-grade inflammation disrupts the tissues that maintain joint health:
- it dries out cartilage
- it reduces collagen repair
- it degrades synovial fluid
- it weakens ligaments and tendons
- it increases stiffness and micro-damage
This manifests as morning stiffness, cracking joints, reduced mobility, slower recovery after physical activity, and early joint degeneration. What many people dismiss as “getting old” often begins with inflammation long before pain becomes obvious.
7. It Disrupts Hormones
Inflammation interferes with nearly every major hormone system:
Insulin: becomes less effective, causing higher blood sugar and increased fat storage.
Thyroid hormones: less T4 converts to active T3, slowing metabolism.
Sex hormones: testosterone, estrogen, and progesterone decline as inflammation rises.
Cortisol: becomes chronically high or unstable, leading to poor sleep, cravings, and abdominal fat.
Leptin: becomes less effective, increasing hunger and reducing fullness signals.
Inflammation creates a cascade effect, once one hormone becomes imbalanced, others follow. Over time, this hormonal disruption drives many of the symptoms that people blame solely on aging.
8. It Damages Your Gut and Microbiome
Chronic inflammation slowly breaks down the integrity of your gut lining. When that lining becomes compromised, small particles, undigested food, toxins, bacterial fragments can seep into the bloodstream. The immune system treats these particles as threats, which triggers even more inflammation.
This cycle leads to:
- bloating
- food intolerances
- IBS-like discomfort
- poor nutrient absorption
- increased autoimmune reactions
- mood instability
- disrupted sleep
Because most of your immune system is located in the gut, anything that destabilizes this system affects nearly every other system in your body.
9. It Drives Autoimmune Conditions
Constant, low-level inflammation keeps the immune system on high alert. Over time, that heightened state can make the immune system lose its ability to distinguish between “self” and “non-self.” When that happens, it starts attacking healthy tissues.
This increases the risk of conditions such as:
- rheumatoid arthritis
- lupus
- Hashimoto’s thyroiditis
- psoriasis
- inflammatory bowel diseases
The global rise in autoimmune disorders mirrors the rise in chronic inflammatory lifestyles, poor diet, stress, disrupted sleep, toxins, and sedentary behavior.
10. It Accelerates Muscle Loss and Reduces Strength
Inflammation interferes with your body’s ability to build and maintain lean muscle. It disrupts muscle protein synthesis and slows recovery after physical activity.
With age, this leads to:
- faster muscle loss
- decreased strength
- reduced balance and coordination
- a slower metabolism
- greater risk of falls and fractures
- reduced ability to recover from workouts
Age-related muscle loss (sarcopenia) is not just a “normal part of aging.” Inflammation is one of the major accelerating factors.
11. It Ages Your Skin
Your skin is one of the most visible places where inflammation shows itself. Inflammatory molecules break down collagen and elastin, the proteins responsible for firmness and elasticity. They also degrade hyaluronic acid, which keeps skin hydrated.
Over time, this results in:
- more fine lines
- deeper wrinkles
- sagging
- uneven pigmentation
- a dull, tired appearance
- slower wound healing
Topical skincare can only do so much. If inflammation is high internally, the skin will continue aging faster regardless of products.
12. It Shrinks Your Energy Levels
When inflammation rises, mitochondrial efficiency drops. These mitochondria are the engines inside your cells, and when they become less efficient, energy production suffers.
This shows up as:
- persistent fatigue
- burnout
- reduced stamina
- weaker gym performance
- brain fog and slow thinking
People often blame age for their low energy, but inflammation is one of the leading culprits.
13. It Impairs Sleep Quality
Inflammation disrupts neurotransmitters and hormones that regulate the sleep–wake cycle. It also increases physical discomfort and can worsen existing sleep disorders.
This leads to:
- trouble falling asleep
- waking up frequently
- poor deep sleep
- early morning waking
- worsening sleep apnea
- feeling unrefreshed even after a full night
And because poor sleep itself increases inflammation, the cycle can spiral unless it’s addressed deliberately.
14. It Affects Sexual and Reproductive Health
Sexual health declines long before most people expect and inflammation is a major driver.
It contributes to:
- reduced libido
- erectile dysfunction
- hormonal imbalance
- painful periods
- faster ovarian aging
- reduced fertility in both men and women
Inflammation affects blood flow, hormone regulation, and tissue health, three pillars of sexual function.
15. It Increases Cancer Risk
Inflammation does not directly “cause” cancer, but it creates biological conditions that make cancer more likely to form and spread. Over time, inflammatory molecules:
- damage DNA
- impair immune cells responsible for detecting abnormal cells
- increase free radical formation
- encourage tumor growth
- accelerate tissue breakdown
This is why long-term inflammation is a common factor in many cancers that develop later in life.
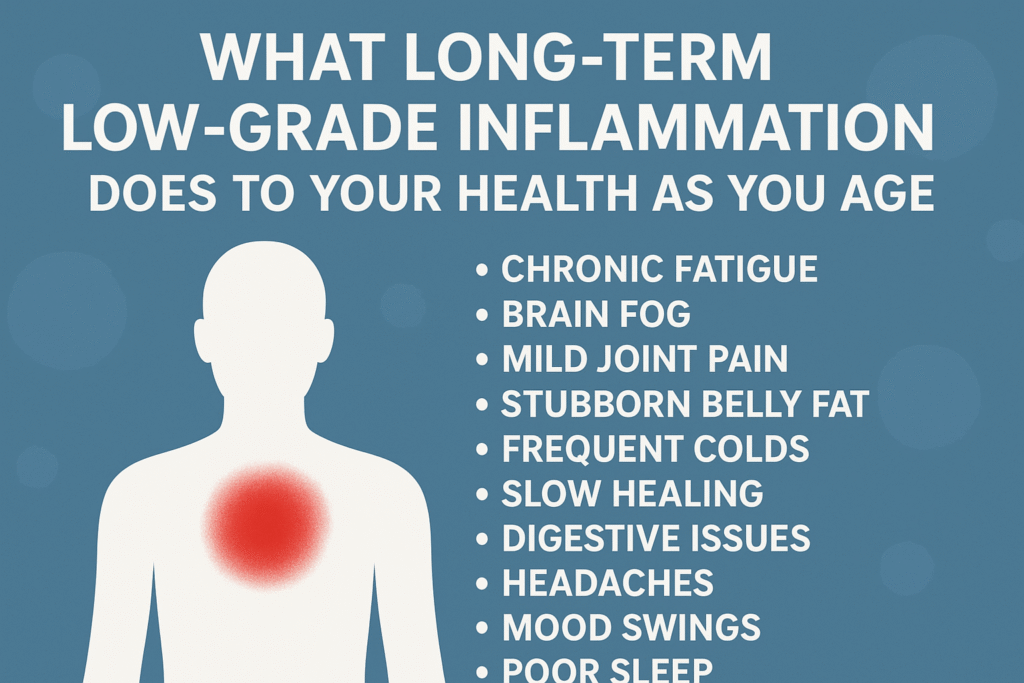
Early Signs You Might Have Low-Grade Inflammation
You won’t see redness or swelling, but your body sends signals. The most common include chronic fatigue, brain fog, mild joint pain, stubborn belly fat, frequent colds, slow healing, digestive issues, headaches, mood swings, poor sleep, high fasting blood sugar, and elevated CRP on blood tests. Most people dismiss these as stress or aging, they aren’t. These are early warnings that your immune system is running hotter than it should.
How to Reduce Low-Grade Inflammation as You Age
You can’t shut inflammation off completely, but you can bring it back to a healthy baseline.
- Prioritize anti-inflammatory nutrition
Build your diet around vegetables, berries, olive oil, fatty fish, turmeric, ginger, nuts, seeds, mushrooms, and green tea. Reduce sugar, ultra-processed foods, refined oils, alcohol, and excessive red meat. - Improve sleep quality
Most adults underestimate how little they actually sleep. Restorative sleep is one of the fastest ways to lower inflammatory markers. - Move daily
Consistent movement matters more than intensity. Even simple post-meal walks significantly reduce inflammation and improve metabolic stability. - Reduce visceral fat
A small reduction in waistline about 5-7% body weight can dramatically decrease inflammatory chemicals released by abdominal fat. - Support gut health
Adequate fiber, probiotics, fermented foods, and reduced alcohol intake help repair the gut lining and calm immune activation. - Manage stress effectively
Controlled breathing, meditation, time in nature, prayer, or journaling all reduce cortisol instability and help regulate inflammation. - Avoid smoking and limit alcohol
Both directly trigger inflammatory pathways and accelerate aging. - Improve metabolic health
Stable blood sugar prevents the cycle where insulin resistance fuels inflammation and inflammation worsens insulin resistance. - Strength training
Muscle tissue is one of your strongest anti-inflammatory assets. Building and preserving it helps regulate blood sugar, hormones, metabolism, and immune function as you age.
Final Truth
Aging itself is not what destroys health, inflammation does.
People don’t suddenly fall apart at 40, 50, or 60 because the body gets old. They unravel because inflammation has been quietly sabotaging their cells, hormones, metabolism, joints, and organs for years, long before symptoms show up. Time is not the enemy,
unchecked inflammation is.
And while you cannot pause the clock, you can take control of the process that makes the clock feel heavier, faster, and more unforgiving than it needs to be.
When you lower chronic inflammation, you change the entire trajectory of your life:
- You age with stability and strength.
- You stay healthier for longer.
- You preserve your energy, stamina, and drive.
- You maintain mental clarity and emotional balance.
- You keep your body resilient instead of fragile.
- You extend the number of years you live without disease, not just the number of years you’re alive.
This is the difference between simply getting older and truly staying well. Aging is unavoidable, inflammaging is optional.
Your future health is not determined by your birthday, it’s determined by the choices you make today to calm the silent fire within. When you reduce inflammation, you don’t just add years to your life, you add quality, vitality, and freedom to every one of them.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowOther Related Blog Post You Might Like:
- 7 Bedtime smoothie for sleep and inflammation
- 10 Powerful Ways to Fix Energy Drops in Your 30s and Regain Vitality Naturally
- 10 Powerful Ways to Fix Energy Drops in Your 30s and Regain Vitality Naturally
- 7 Shocking Risks of Too Much Protein for Non-Athletes: What You Must Know
- 10 Proven Ways Intermittent Fasting Improves Hormone Balance and Your Biological Clock
- Is Sleeping with the Light On Bad for You? 7 Hidden Health Risks Explained
- 7 Real Consequences of Holding Pee Too Long: What You Need to Know
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


