⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
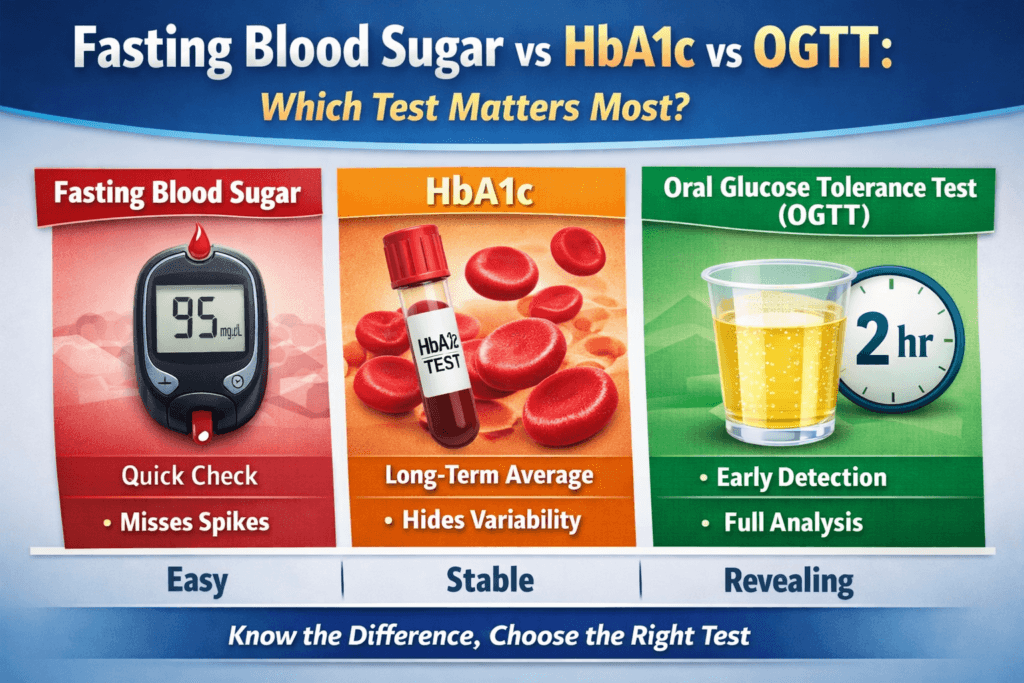
Fasting Blood Sugar vs HbA1c vs OGTT: 7 Critical Differences Every Patient Must Know
Diabetes and prediabetes are often presented as binary conditions, you either have them or you do not, that framing is convenient, but it is medically inaccurate. Glucose regulation is not an on oroff switch. It is a continuum, shaped by hormonal signaling, organ function, genetics, lifestyle, and time. Long before diabetes is diagnosed, metabolic control begins to fracture quietly, often without obvious symptoms.
This complexity is the reason modern medicine does not rely on a single laboratory value to assess glucose metabolism, instead, three primary tests are used, each designed to interrogate a different physiological layer of glucose control:
Fasting Blood Sugar (FBS), which reflects baseline glucose regulation after an overnight fast.
HbA1c (glycated hemoglobin), which estimates average glucose exposure over several months.
Oral Glucose Tolerance Test (OGTT), which challenges the body with a glucose load to reveal how well it responds under metabolic stress.
On paper, these tests appear interchangeable, in practice they are not. Patients are often told one number is normal while another is borderline or abnormal. This leads to understandable confusion, which test is more accurate, why results conflict, and which number truly represents risk.
The uncomfortable medical reality is that no single test tells the full story, each test captures a different failure point in glucose regulation. One may appear normal while another already signals pathology, when these differences are misunderstood or ignored, early disease is missed, reassurance is falsely given, and intervention is delayed until damage is already underway.
This article examines what each test truly measures at a physiological level, what each one fails to detect, why discordant results are common rather than rare, and which test matters most depending on the clinical question being asked. The goal is not to crown a single best test, but to clarify how glucose dysregulation actually unfolds and how to detect it before it becomes irreversible.
Understanding Blood Glucose Regulation: Why One Test Is Never Enough
Blood glucose regulation is the result of several biological systems operating in constant coordination. When any one of these systems begins to fail, glucose control deteriorates often in subtle ways that standard testing can miss.
Key components of glucose regulation include:
Insulin secretion from the pancreas, which determines how effectively glucose can be moved out of the bloodstream and into cells. Insulin sensitivity in muscle, fat, and liver tissue, which governs how responsive those tissues are to insulin’s signal.
Glucose production by the liver, which continues even during fasting and must be carefully suppressed by insulin. Incretin hormones released from the gut, which amplify insulin release after meals and modulate postprandial glucose levels.
Renal glucose handling by the kidneys, which determines when excess glucose begins to spill into the urine.
Because these systems are influenced by circadian rhythms, food intake, physical activity, stress hormones, illness, and sleep quality, blood glucose levels are inherently dynamic. They rise after meals, fall during sleep, surge during stress, and fluctuate from hour to hour even in healthy individuals.
Each diagnostic test used in diabetes assessment captures only a narrow window into this continuously shifting process. No single measurement can reflect the full complexity of glucose metabolism. For this reason, relying on one test in isolation is physiologically unsound and clinically risky.
1. Fasting Blood Sugar (FBS)
What Fasting Blood Sugar Measures
Fasting Blood Sugar measures plasma glucose concentration after a minimum of eight hours without caloric intake, most commonly in the early morning.
Physiologically, fasting glucose reflects:
- Baseline insulin secretion in the absence of food stimuli,
- overnight hepatic glucose output, which is normally suppressed by insulin.
- Fasting insulin resistance, particularly at the level of the liver.
It primarily evaluates how well the body maintains glucose control in a resting, unstressed state.
Diagnostic Thresholds
Fasting Glucose (mg/dL) | Interpretation |
Below 100 | Normal |
100-125 | Prediabetes (impaired fasting glucose) |
126 or higher | Diabetes (requires confirmation) |
Strengths of Fasting Blood Sugar
Fasting glucose testing is simple, inexpensive, and widely accessible. It is effective at identifying more advanced disturbances in basal glucose regulation and is commonly used for routine monitoring in individuals with established diabetes, because it is easy to perform and standardized across laboratories, it remains a practical clinical tool.
Major Limitations of Fasting Blood Sugar
Despite its convenience, fasting glucose is a poor detector of early disease. Many individuals maintain normal fasting levels while experiencing substantial glucose elevations after meals, where much of the metabolic damage actually occurs.
Fasting glucose represents a single time point and provides no information about daily glucose variability or postprandial excursions. It is also sensitive to external influences such as sleep deprivation, acute stress, illness, corticosteroid release, and the dawn phenomenon, all of which can distort results.
A normal fasting glucose does not indicate normal glucose metabolism. It only indicates that fasting control has not yet failed.
Clinical Bottom Line on FBS
Fasting blood sugar is useful but incomplete. When interpreted in isolation, it frequently underestimates the presence and severity of metabolic dysfunction, particularly in early-stage disease.
2. HbA1c (Glycated Hemoglobin)
What HbA1c Measures
HbA1c represents the proportion of hemoglobin molecules in circulating red blood cells that have glucose irreversibly bound to them because red blood cells survive for approximately 120 days, HbA1c reflects weighted average blood glucose exposure over the preceding two to three months.
Rather than capturing momentary glucose levels, HbA1c summarizes cumulative exposure over time.
Diagnostic Thresholds
HbA1c (%) | Interpretation |
Below 5.7 | Normal |
5.7-6.4 | Prediabetes |
6.5 or higher | Diabetes |
Strengths of HbA1c
HbA1c provides a stable, long-term overview of glycemic exposure and does not require fasting. It is less influenced by short-term variability and correlates strongly with the risk of chronic microvascular complications, including diabetic retinopathy, nephropathy, and neuropathy.
For this reason, HbA1c is particularly valuable for tracking disease progression, evaluating long-term treatment effectiveness, and estimating cumulative risk.
Also Read: 10 Proven Tips on How to Interpret Hemoglobin A1c Levels Accurately
Important Limitations of HbA1c
HbA1c does not reflect glucose variability. Two individuals with the same HbA1c may have radically different glucose profiles, one relatively stable, the other characterized by frequent post-meal spikes and hypoglycemic dips.
It is also relatively insensitive to early postprandial hyperglycemia, which can drive vascular injury before average glucose levels rise appreciably. Accuracy is further compromised in conditions that affect red blood cell lifespan or hemoglobin structure, including anemia, hemoglobinopathies, chronic kidney disease, recent blood loss, pregnancy, and rapid red cell turnover. Genetic and ethnic differences can alter HbA1c independently of true glucose exposure.
Clinical Bottom Line on HbA1c
HbA1c is a powerful tool for assessing long-term risk and monitoring established disease. However, it is insufficient as a standalone screening test and frequently fails to identify early or fluctuating glucose abnormalities.
3. Oral Glucose Tolerance Test (OGTT)
What OGTT Measures
The Oral Glucose Tolerance Test evaluates the body’s ability to manage a controlled glucose challenge. Rather than assessing glucose levels in a resting state, OGTT intentionally stresses the metabolic system to reveal weaknesses that remain hidden under fasting conditions.
Standard procedure involves:
- An overnight fast to establish baseline metabolic conditions.
- Measurement of fasting plasma glucose.
- Ingestion of a standardized 75-gram oral glucose load.
- Measurement of plasma glucose at two hours to assess clearance efficiency.
Extended protocols may include additional measurements at 30 and 60 minutes. These intermediate values provide deeper insight into early insulin secretion, peak glucose excursions, and delayed glucose clearance, patterns that are highly predictive of future diabetes and cardiovascular risk.
OGTT therefore examines not only whether glucose rises, but how quickly and effectively the body responds to that rise.
Diagnostic Thresholds (Two-Hour Value)
Two-Hour Glucose (mg/dL) | Interpretation |
Below 140 | Normal |
140-199 | Prediabetes (impaired glucose tolerance) |
200 or higher | Diabetes |
Strengths of OGTT
OGTT is the most sensitive clinical test for detecting early abnormalities in glucose regulation. It identifies post-meal hyperglycemia and insulin resistance long before fasting glucose or HbA1c levels become abnormal.
Because most glucose exposure occurs after eating, OGTT directly evaluates the metabolic state in which damage is most likely to occur. It is particularly effective at uncovering early pancreatic beta-cell dysfunction and peripheral insulin resistance.
OGTT is also the diagnostic gold standard for gestational diabetes and remains one of the strongest predictors of progression from prediabetes to overt diabetes. In many individuals, OGTT reveals clinically significant disease that would otherwise remain undiagnosed using standard screening tests.
Limitations of OGTT
Despite its diagnostic power, OGTT is underutilized in routine practice. The test is time-consuming, requires patient preparation, and involves remaining in a clinical setting for several hours. The glucose solution is unpleasant for many patients and can cause nausea or lightheadedness.
Results are also sensitive to recent illness, physical activity, medications, and improper fasting, making strict adherence to protocol essential.
These practical limitations, rather than physiological shortcomings, explain why OGTT is less commonly performed, not because it is less informative, but because it is less convenient.
Clinical Bottom Line on OGTT
OGTT provides the most complete picture of early and hidden glucose dysregulation. Although inconvenient, it is unmatched in its ability to detect disease at a stage when intervention is most effective.
Direct Comparison of the Three Tests
Feature | Fasting Blood Sugar | HbA1c | OGTT |
Measures fasting control | Yes | Partial | Yes |
Measures post-meal control | No | No | Yes |
Detects early diabetes | Poor | Moderate | Strong |
Convenience | High | High | Low |
Predicts long-term complications | Limited | Strong | Moderate |
Affected by anemia | No | Yes | No |
Which Test Matters Most?
There Is No Single Winner
The clinical value of each test depends on the question being asked. Glucose dysregulation does not occur uniformly, and different tests identify different failure points within the metabolic system.
For Early Detection
OGTT matters most when the goal is identifying early insulin resistance or post-meal hyperglycemia. A significant number of individuals with normal fasting glucose and normal HbA1c already demonstrate abnormal OGTT results, indicating early disease that would otherwise go unnoticed.
For Long-Term Risk Assessment
HbA1c is most useful for estimating cumulative glucose exposure and predicting the likelihood of chronic complications. It remains the strongest single marker for long-term microvascular risk.
For Routine Monitoring
In individuals with established diabetes, fasting glucose combined with HbA1c provides practical guidance for treatment adjustment and trend monitoring over time.
Why Test Results Often Conflict
Conflicting results do not imply laboratory error. They reflect different stages and patterns of metabolic failure.
A common scenario involves normal fasting glucose, normal HbA1c, and an abnormal OGTT. This pattern indicates preserved fasting control but impaired glucose handling after meals, a hallmark of early insulin resistance and declining beta-cell reserve.
Understanding this distinction is critical, it explains why individuals may be reassured prematurely and why disease progression often occurs silently for years.
The Dangerous Myth of Normal HbA1c Means No Problem
Post-meal glucose spikes generate oxidative stress, endothelial dysfunction, low-grade inflammation, and increased cardiovascular risk well before HbA1c reaches diagnostic thresholds.
Relying solely on HbA1c delays diagnosis and intervention until cumulative damage has already occurred, by the time HbA1c rises, the disease process is no longer early.
What Intelligent Testing Looks Like
In individuals with established risk factors, glucose assessment should never rely on a single laboratory value. Family history of diabetes, excess body weight, polycystic ovary syndrome, prior gestational diabetes, and existing cardiovascular disease all signal an increased likelihood of early and atypical glucose dysregulation.
In these populations, testing must be layered rather than selective.
HbA1c and fasting blood glucose should serve as baseline assessments, providing information about long-term exposure and resting metabolic control. These tests establish trends and identify advanced abnormalities, but they do not reliably exclude early disease.
When results are borderline, when symptoms persist despite normal values, or when clinical risk is high in the presence of reassuring averages, an Oral Glucose Tolerance Test should be added. OGTT exposes defects in post-meal glucose handling that fasting and averaged measurements frequently miss, particularly in the early stages of insulin resistance and beta-cell dysfunction.
Intelligent testing prioritizes physiology over convenience. It accepts that normal numbers do not always mean normal metabolism and that early detection requires challenging the system, not merely observing it at rest.
The goal is not to accumulate more data, but to ask the right metabolic questions at the right time before silent dysfunction becomes irreversible disease.
Final Truth
Fasting glucose is simple to obtain, but it only reflects metabolic control at rest. HbA1c offers stability and long-term perspective, yet it averages away the very fluctuations where early damage begins. OGTT is inconvenient by design, but that inconvenience is precisely what makes it revealing.
When the priority is ease, HbA1c is adequate, when the priority is confidence, OGTT cannot be excluded. When the priority is early detection, OGTT is the test that matters most.
Diabetes does not start at a laboratory threshold. It starts when the body can no longer manage glucose under normal physiological stress. By the time averages rise and fasting numbers fail, dysfunction has already been present for years.
The purpose of testing is not to confirm disease once it is obvious, but to uncover failure while it is still silent. Only the right test, used at the right time, exposes that reality.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Blog Post:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- How Blood Sugar Is Regulated in the Body: 10 Key Mechanisms Explained
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- Early Warning Signs of Diabetes Most People Ignore: 10 Subtle Symptoms You Must Know
- Unexplained Weight Loss or Gain in Diabetes: 11 Shocking Reasons It Happens
- 10 Critical Insights Into Frequent Urination and Thirst in Diabetes: The Physiology Behind Classic Symptoms
- 12 Powerful Early Signs of Insulin Resistance You Should Watch and How to Fix Them
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


