Early Warning Signs of Diabetes Most People Ignore: 10 Subtle Symptoms You Must Know
⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
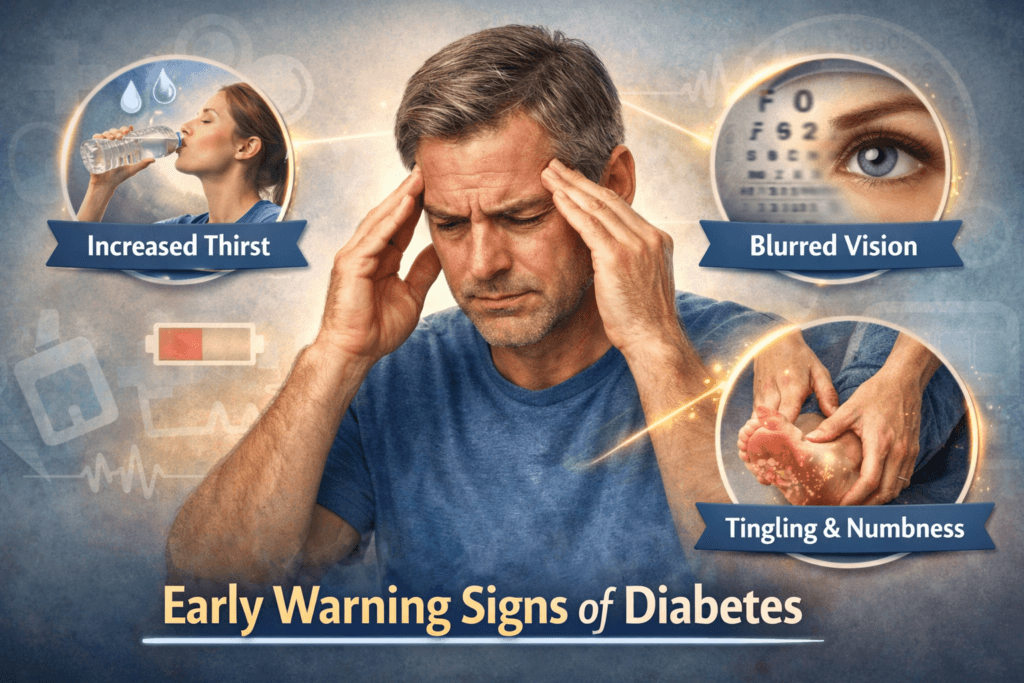
Many people assume diabetes is obvious, weight gain, constant thirst, or frequent urination. In reality, it often begins quietly, hidden behind the rhythms of daily life and easily dismissed complaints. Subtle shifts in energy, mood, focus, or even sleep patterns can be early signals that your body is struggling with glucose regulation long before a formal diagnosis.
These early whispers are easy to overlook because they feel ordinary, intermittent, or explainable by stress, diet, or lifestyle. Ignoring them, however, allows metabolic dysfunction to progress silently, sometimes for years, causing damage that may only become apparent once complications emerge.
This article highlights the early warning signs of diabetes that are often missed, explaining why they occur, what they reveal about your body’s health, and why paying attention to them can be the difference between early intervention and long-term complications.
Why Early Diabetes Is So Easy to Miss
The human body is remarkably adept at maintaining balance, even when something begins to go wrong. When insulin action starts to falter, whether due to resistance in tissues or declining pancreatic secretion, the body activates compensatory mechanisms to keep blood glucose levels within a survivable range. These adaptations can mask the early progression of diabetes, making it nearly invisible to both patients and sometimes even clinicians.
As a result:
- Blood sugar may remain borderline for months or even years.
- Symptoms appear intermittently rather than constantly, making them easy to dismiss.
- The body adapts just enough to maintain day-to-day function, giving the illusion that all is normal.
Because life continues relatively unaffected, many people assume that nothing serious is happening. Yet beneath the surface, subtle metabolic dysfunction is quietly advancing, laying the groundwork for more serious complications down the line.
1. Persistent Fatigue That Doesn’t Match Your Lifestyle
One of the earliest and most commonly overlooked signs of diabetes is unexplained, persistent fatigue. This is not ordinary tiredness after a long day, it’s a deep, chronic depletion of energy that doesn’t improve with rest or sleep. Although glucose may be abundant in the bloodstream, insulin resistance or deficiency prevents it from entering cells efficiently, muscle and fat cells are surrounded by fuel yet remain starved for energy. The brain, sensing this cellular “starvation,” interprets it as exhaustion.
This fatigue is not about laziness, poor sleep, or overwork, it reflects a fundamental issue in how the body delivers energy to cells.
Why People Ignore It:
- They attribute it to work stress or busy schedules.
- They assume sleep deprivation or burnout is to blame.
- Chronic tiredness becomes normalized, accepted as part of life.
Unchecked, this fatigue becomes the new baseline, allowing diabetes to progress silently while the body struggles to compensate.
2. Increased Thirst and Subtle Dehydration
Excessive thirst is often considered a classic symptom of diabetes, but early on, it is usually subtle and easy to overlook.
People might notice:
- Drinking water more frequently than usual.
- A persistent dry mouth or mild dehydration.
- A preference for cold or sweet beverages.
As blood glucose levels rise, the kidneys attempt to remove the excess sugar via urine. Glucose pulls water along with it, increasing fluid loss, even before noticeable polyuria (frequent urination) develops, mild dehydration can trigger the sensation of thirst.
Why It’s Dismissed:
- Hot weather or sweating is blamed.
- Increased physical activity is assumed to require more water.
- People tell themselves, “I just don’t drink enough water.”
In reality, this subtle thirst is a sign that the body is struggling to maintain osmotic balance and that glucose regulation is already impaired.
3. Frequent Urination Especially at Night
Frequent urination is another hallmark symptom of early diabetes, but it often presents subtly, making it easy to overlook.
Common early patterns include:
- Waking up once or twice in the middle of the night to urinate.
- Passing larger urine volumes than usual.
- Experiencing increased urgency without signs of infection.
What This Signals:
The kidneys have a threshold for glucose reabsorption. Once blood sugar slightly exceeds this threshold, glucose spills into the urine, drawing water along with it. This effect is especially noticeable at night because fluid intake is low, yet urine production increases.
Why People Ignore It
- Aging is often blamed as the cause of nighttime urination.
- Consumption of caffeine or alcohol is assumed to be responsible.
- People may attribute it to a small bladder or other benign causes.
Even when subtle, this is one of the earliest measurable physiological changes of diabetes. Recognizing it can be a critical step toward early detection and intervention, potentially preventing long-term complications.
4. Increased Hunger Despite Eating Normally
A paradoxical but common early sign of diabetes is persistent hunger, even after eating normally.
People may notice:
- Feeling hungry shortly after meals.
- Cravings for carbohydrates or sweet foods.
- Difficulty feeling full or satisfied.
Insulin resistance or insufficient insulin prevents glucose from entering cells efficiently. Even when you’ve eaten enough, your cells remain starved for energy. The brain senses this energy deficit and signals hunger to encourage more intake. In other words, you are eating enough, but your body cannot access the fuel it needs.
Why It’s Often Misinterpreted:
- People assume it’s stress eating.
- Some blame a naturally high metabolism.
- Exercise-related hunger is also a common explanation.
This type of hunger is metabolic, not behavioral. Ignoring it allows the underlying insulin resistance to worsen over time.
5. Brain Fog and Difficulty Concentrating
Cognitive changes are rarely associated with metabolic disorders, yet the brain is highly dependent on stable glucose levels for energy.
Early signs may include:
- Trouble focusing or sustaining attention.
- Slower processing of information.
- Memory lapses or forgetfulness.
- Reduced mental endurance, especially during work or study.
The Underlying Mechanism
Fluctuating blood sugar levels impair the brain’s energy supply. Repeated episodes of hyperglycemia also trigger oxidative stress and subtle inflammation, which can affect neuronal function and signaling.
Why It’s Often Dismissed:
- Symptoms are attributed to anxiety or stress.
- People blame depression or mood changes.
- Overwork or poor sleep is a common assumption.
In reality, these cognitive changes are the brain’s response to unstable fuel delivery, signaling early metabolic imbalance.
6. Blurred Vision That Comes and Goes
Vision changes in early diabetes are often intermittent rather than constant, making them easy to overlook.
People may notice:
- Blurred vision after meals.
- Difficulty focusing on nearby or distant objects.
- Day-to-day fluctuations in clarity of vision.
High blood glucose alters the osmotic balance in the lens of the eye, changing its shape and refractive index. This temporarily affects how light is focused, leading to blurred vision. Although reversible at this stage, repeated episodes may precede more serious diabetic eye complications later on.
Why It’s Often Ignored:
- Attributing blurriness to screen strain or fatigue.
- Thinking new glasses are needed.
- Dismissing it as occasional tired eyes.
Recognizing these subtle changes early allows timely intervention to protect long-term eye health.
7. Slow Healing of Minor Cuts and Infections
Another early warning sign is delayed healing. Small cuts, scrapes, or minor infections take longer than usual to recover.
Examples include:
- Minor cuts lingering for weeks.
- Frequent skin infections.
- Recurrent fungal infections, such as athlete’s foot or yeast infections.
What’s Driving It:
Chronic hyperglycemia impairs several aspects of the body’s repair mechanisms:
- Reduced immune cell efficiency, making it harder to fight infections.
- Slower collagen synthesis, which is necessary for tissue repair.
- Microvascular circulation impairment, limiting nutrient delivery to injured tissues.
Why It’s Often Minimized:
- People assume, “I just heal slowly.”
- Poor circulation is blamed.
- Hygiene or environmental factors are considered responsible.
Delayed healing is a sensitive indicator of early metabolic dysfunction and should not be ignored.
8. Tingling or Numbness in Hands and Feet
Neuropathy or nerve damage, is often considered a late complication of diabetes but early nerve dysfunction can appear long before diagnosis.
Early sensations may include:
- Mild tingling or pins-and-needles.
- Occasional numbness or reduced sensation in extremities.
- Subtle changes in touch or temperature perception.
High blood sugar damages small nerve fibers and the blood vessels that supply them. Early injury is usually subtle and reversible if addressed promptly.
Why It’s Often Ignored
- Attributing sensations to sitting posture or minor pressure.
- Assuming vitamin deficiencies are to blame.
- Thinking it’s temporary nerve compression or fatigue.
These early nerve symptoms are warning signs, not random or harmless sensations, and they indicate that metabolic stress is affecting the nervous system.
9. Darkened Skin Folds (Acanthosis Nigricans)

Dark, velvety patches of skin particularly on the neck, armpits, or groin can be an early, visible marker of insulin resistance.
What It Indicates
Chronically high insulin levels stimulate abnormal skin cell growth and increased pigmentation, producing these characteristic patches. This skin change often appears years before a formal diabetes diagnosis, making it an early warning sign that should not be ignored.
Why It’s Often Overlooked
- People assume it is genetic or hereditary.
- It is mistakenly attributed to poor hygiene.
- Cosmetic concerns are seen as the only issue, rather than a sign of metabolic stress.
Acanthosis nigricans is one of the clearest external indicators of underlying insulin resistance and early metabolic dysfunction.
10. Subtle Weight Changes Without Effort
Early diabetes does not always lead to obvious weight gain. Some individuals experience unintentional weight loss or subtle shifts in body composition.
People may notice:
- Losing weight without changing diet or exercise habits.
- Reduction in muscle mass.
- Redistribution of fat, particularly around the abdomen.
When glucose cannot be utilized effectively, the body turns to fat and muscle for energy. This catabolic state may occur even in type 2 diabetes and reflects the body’s struggle to maintain energy homeostasis.
Why It’s Often Misread:
- Mistaken for successful dieting or exercise results.
- Attributed to stress, illness, or lifestyle changes.
- Misunderstood as harmless “normal fluctuations.”
Weight loss in this context is a sign of metabolic stress, not necessarily health improvement.
Why These Signs Matter More Than Blood Sugar Alone
Many people rely solely on fasting glucose tests to assess diabetes risk. While useful, these tests can miss early metabolic dysfunction.
Early diabetes often includes:
- Post-meal glucose spikes that occur even when fasting glucose is normal.
- Insulin resistance with compensatory hyperinsulinemia.
- Symptoms reflecting physiological stress that lab values may not yet capture.
Recognizing these subtle signs allows for earlier detection and intervention, long before irreversible damage occurs.
The Cost of Ignoring Early Warning Signs
Unchecked metabolic dysfunction can lead to serious, long-term complications:
- Progressive failure of pancreatic beta cells.
- Vascular damage, increasing cardiovascular risk.
- Nerve injury (neuropathy), affecting sensation and mobility.
- Kidney stress and potential chronic kidney disease.
- Heightened risk of heart attacks and strokes.
By the time diabetes is officially diagnosed, damage has often already begun, emphasizing the importance of early recognition.
When to Take Action:
You should not wait for dramatic or severe symptoms. Early evaluation is warranted if multiple subtle signs appear, especially in the presence of risk factors such as:
- Family history of diabetes.
- Central obesity or increased abdominal fat.
- Sedentary lifestyle.
- History of gestational diabetes or other metabolic conditions.
Early intervention is prevention, not overreaction. Detecting and addressing these signs promptly can slow progression, protect organs, and significantly improve long-term health outcomes.
Final Perspective
Diabetes rarely strikes suddenly, instead it unfolds over a long, quiet phase during which the body compensates, adapts, and struggles silently to maintain balance. By the time a formal diagnosis is made, metabolic disruptions may have been quietly progressing for years.
The early warning signs fatigue, subtle thirst, increased hunger, brain fog, tingling in the extremities, darkened skin folds, and minor weight changes are neither rare nor mysterious. They are common signals that the body is under metabolic stress, yet they are routinely dismissed as trivial, lifestyle-related, or age-associated.
Paying attention to these signs is not about fear or alarmism. It is about respecting the body’s physiology and understanding its subtle messages. Recognizing them early gives you the chance to act through lifestyle adjustments, monitoring, or medical evaluation before irreversible damage occurs.
Ignoring these signals does not halt disease progression, it only allows hidden dysfunction to advance unchecked. Understanding them, interpreting them correctly, and taking timely action can change the trajectory of your health, preserving organ function and preventing serious complications.
In essence, early recognition transforms diabetes from a silent threat into a manageable condition and your body’s early warnings are the roadmap.
💡 Expert Guidance at Your Fingertips
Speak with a licensed doctor from MuseCare Consult and get actionable advice for your health questions, labs, or medications, all online and secure.
💬 Start Your ConsultationRelated Blog Post:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- How Blood Sugar Is Regulated in the Body: 10 Key Mechanisms Explained
- 10 Proven Benefits of Nutritional Counseling for Diabetes Management
- 10 Sneaky Symptoms of Prediabetes in Women Over 40 You Can’t Ignore
- 10 Proven Tips on How to Interpret Hemoglobin A1c Levels Accurately
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


