12 Powerful Ways to Tell Tension Headache vs Migraine: Accurate Diagnosis Guide
Headaches affect millions of people every day, yet many struggle to understand what type they are actually experiencing. Pain in the head is often grouped under one label, but tension headaches and migraines are fundamentally different conditions. When these two are confused, people end up treating the wrong problem, relying on ineffective medications, or delaying proper medical care.
The difference between a tension headache and a migraine is not a matter of terminology, it determines how the headache behaves, how severe it becomes, how long it lasts, and how it should be treated. Correct identification is the foundation of effective management and long term relief.
This guide focuses exclusively on how to recognize and diagnose tension headaches versus migraines by examining symptoms, pain patterns, triggers, and established clinical criteria, it provides a clear framework for distinguishing between the two and understanding when further medical evaluation is necessary.
Why Correct Identification Matters
Correctly identifying the type of headache is essential because tension headaches and migraines respond to very different management strategies. When a migraine is treated as a simple tension headache, pain relief is often incomplete or short lived, on the other hand, treating a tension headache with migraine specific medications can expose a person to unnecessary drugs without meaningful benefit, misidentification commonly leads to several problems.
Symptoms remain poorly controlled, causing repeated pain episodes that affect daily life, people may begin using painkillers too frequently, which increases the risk of medication overuse headaches. Migraines may progress from episodic to chronic because the underlying condition is not recognized early. In some cases, anxiety increases, prompting unnecessary imaging studies despite the absence of warning signs.
The key to proper diagnosis is not how intense the pain feels in a single moment, it is the overall pattern of the headache, including how it starts, how it behaves, and what symptoms accompany it.
Key Differences at a Glance
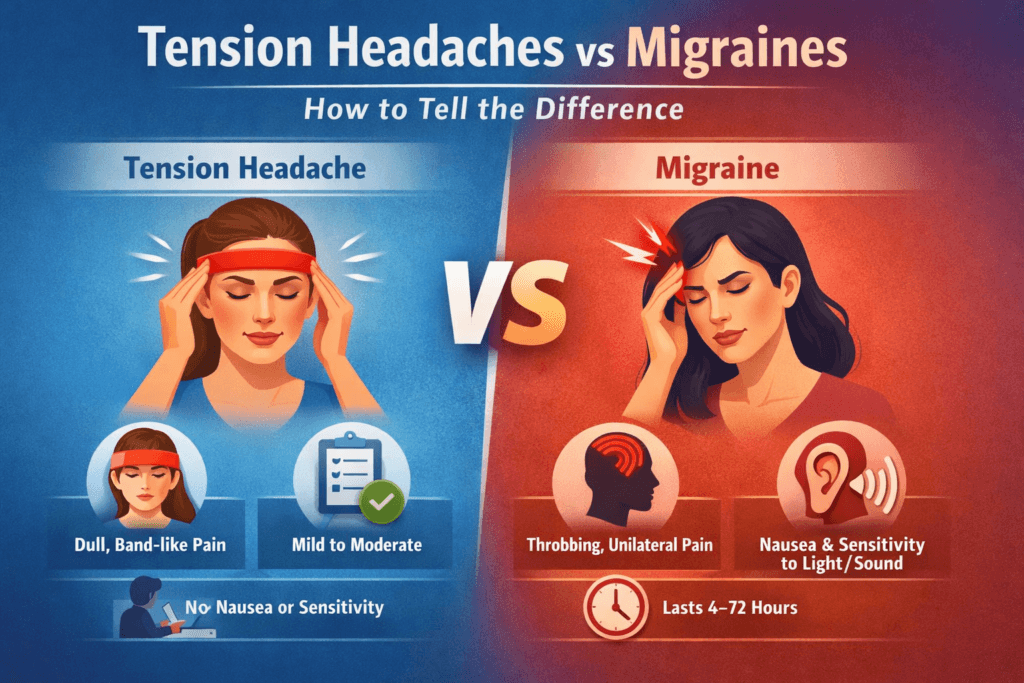
Tension headaches and migraines differ in several consistent and clinically meaningful ways. Tension headaches typically produce a dull, tight, pressure-like discomfort, while migraines are more often described as throbbing or pulsating. The pain of a tension headache usually affects both sides of the head and feels like a band or pressure around the skull. Migraine pain is more likely to affect one side, although it can alternate sides between attacks.
Intensity also helps distinguish the two. Tension headaches are usually mild to moderate and often allow people to continue their normal activities. Migraines tend to be moderate to severe and frequently force individuals to stop working, rest in a dark room, or lie down.
Physical activity provides another important clue, normal movement, walking, or climbing stairs does not worsen tension headaches. Migraine pain, however, typically intensifies with routine physical activity.
Associated symptoms strongly favor migraine when present. Nausea is common in migraines and absent in tension headaches, sensitivity to light and sound is minimal or absent in tension headaches but prominent in migraines. Aura, which consists of temporary neurological symptoms, never occurs with tension headaches and occurs in a subset of migraine sufferers. Duration also differs, with tension headaches lasting from minutes to hours and migraines lasting anywhere from four to seventy two hours if untreated.
This comparison provides orientation, but accurate diagnosis depends on a deeper understanding of each condition.
Understanding Tension Headaches
What Is a Tension Headache?
Tension headache is the most common primary headache disorder worldwide. It is associated with sustained muscle activation, stress, poor posture, and altered pain processing within the nervous system. Contrary to older beliefs, it is not caused by blood vessel changes.
Although muscle tension plays a role, it does not fully explain the condition, over time, the brain becomes more sensitive to pain signals coming from the head, neck, and scalp. This heightened sensitivity lowers the threshold at which discomfort is perceived as pain.
Typical Pain Characteristics
The pain of a tension headache is usually described as tight, pressing, squeezing, or heavy, unlike migraine pain, it does not throb or pulse. The sensation is steady and constant.
People often describe it as feeling like a tight band wrapped around the head, pressure behind the eyes, or the sensation of wearing a helmet that is too small. These descriptions are remarkably consistent across patients and are an important diagnostic feature.
Location of Pain
Tension headache pain is almost always bilateral, meaning it affects both sides of the head equally. Common areas involved include the forehead, temples, back of the head, and upper neck.
The pain does not shift from one side to the other during an episode, this stable, symmetrical distribution helps differentiate tension headaches from migraines.
Intensity and Impact on Daily Life
Tension headaches are typically mild to moderate in intensity. While uncomfortable, they usually do not prevent normal daily activities, many people continue working, studying, or performing household tasks despite the discomfort.
This ability to function despite pain is a key diagnostic clue. When a headache consistently disrupts routine activity or forces rest, migraine becomes more likely.
Associated Symptoms
Tension headaches do not produce nausea or vomiting, significant sensitivity to light or sound is also absent.
At most, a person may experience mild sensitivity to either light or sound, but never both at the same time. The presence of combined light and sound sensitivity strongly argues against tension headache.
Duration and Frequency
A tension headache can last anywhere from thirty minutes to several hours. In some cases, especially in chronic tension headache, the discomfort may persist throughout the day.
Frequency is used to classify the condition, episodic tension headaches occur fewer than fifteen days per month, chronic tension headaches occur on fifteen or more days per month for at least three consecutive months. Chronic cases are often associated with long term stress, posture problems, and central pain sensitization.
Triggers and Patterns
Tension headaches commonly develop in response to prolonged physical or mental strain. Typical triggers include extended sitting, poor posture, prolonged screen use, emotional stress, jaw clenching, and inadequate sleep.
The pain often builds gradually as the day progresses rather than appearing suddenly, many people notice worsening discomfort in the afternoon or evening after hours of sustained muscle tension or mental fatigue.
Recognizing these patterns is essential for accurate identification and effective long term management.
Understanding Migraines
What Is a Migraine?
A migraine is a neurological disorder that goes beyond the typical headache, it arises from abnormal brain signaling, changes in neurotransmitter activity, and heightened sensory processing in the nervous system. While pain is the most recognized symptom, migraines involve a spectrum of neurological and systemic manifestations, including visual, sensory, and gastrointestinal disturbances.
Migraines are not caused by simple tension or stress alone, they are a complex brain disorder that affects how the nervous system perceives and processes pain. Recognizing this distinction is essential for effective management and appropriate treatment.
Typical Pain Characteristics
Migraine pain has distinctive qualities that differentiate it from tension headaches. The pain is often described as:
- Throbbing
- Pulsating
- Beating
The intensity of migraine pain is typically moderate to severe and can significantly disrupt daily life. Common effects include:
- Inability to continue work or daily activities
- The need to lie down in a dark, quiet room
- Difficulty concentrating or thinking clearly
Unlike tension headaches, migraine pain is dynamic, often increasing in intensity over hours and responding differently to movement and external stimuli.
Location of Pain
Migraines most often affect one side of the head (unilateral pain), although the side may vary between attacks. Common locations include:
- One temple
- Behind one eye
- Front or side of the head
Bilateral migraines do occur, but they are less common and often present with classic migraine-associated symptoms to confirm the diagnosis. Recognizing the location and pattern of pain over multiple attacks can help differentiate migraines from other headache types.
Effect of Physical Activity
One of the most reliable diagnostic features of migraine is the exacerbation of pain with routine physical activity. Activities that are typically tolerated during a tension headache, such as walking, climbing stairs, or bending over, often worsen migraine pain. This is a key factor in clinical evaluation and helps distinguish migraines from other headache disorders.
Associated Symptoms
Migraines are rarely isolated to head pain alone. They are almost always accompanied by other symptoms, which can include:
- Nausea or vomiting
- Sensitivity to light (photophobia)
- Sensitivity to sound (phonophobia)
- Sensitivity to smell (osmophobia)
At least one of these associated symptoms is typically present during a migraine episode. The combination of moderate to severe headache with these symptoms helps clinicians differentiate migraines from tension headaches or other headache disorders.
Duration
Untreated migraine attacks usually last between 4 and 72 hours. The pain generally develops gradually, reaches a peak, and resolves slowly. Short headaches are less likely to be migraines unless medication is taken early, which can abort or shorten an attack. Understanding the typical duration is critical for both diagnosis and treatment planning.
Migraine Aura: A Distinctive Feature
What Is Aura?
Aura consists of reversible neurological symptoms that occur before or during a migraine attack. While not all migraines are accompanied by aura, it is a defining feature when present, tension headaches never involve aura.
Common Aura Symptoms
Aura typically lasts between 5 and 60 minutes and may include:
Visual disturbances:
- Zigzag lines
- Flashing lights
- Temporary blind spots
Sensory changes:
- Tingling or numbness in the face, hands, or limbs
- Speech difficulties, such as slurred or slowed speech
Aura signals cortical and sensory involvement in the brain and provides a clear clinical marker for migraine diagnosis.
Why Aura Matters
The presence of aura has important implications beyond diagnosis:
- Medication choices: Certain treatments are more effective in patients with aura.
- Stroke risk considerations: Migraine with aura has a slightly increased risk of cerebrovascular events, affecting clinical management.
- Hormonal treatment decisions: The presence of aura may influence the safety of hormonal contraception or replacement therapy.
Identifying aura is therefore critical for both acute management and long-term planning.
Diagnostic Criteria Used by Clinicians
Healthcare professionals rely on standardized guidelines, such as the International Classification of Headache Disorders, to ensure accurate diagnosis.
Tension Headache Diagnostic Criteria
Diagnosis requires:
- At least 10 prior episodes
- Headache lasting between 30 minutes and 7 days
- At least two of the following:
- Bilateral location
- Pressing or tightening quality
- Mild to moderate intensity
- Not aggravated by routine physical activity
- Bilateral location
Additionally:
- No nausea or vomiting
- No more than one of either photophobia or phonophobia
Migraine Diagnostic Criteria
Diagnosis requires:
- At least 5 previous attacks
- Headache lasting between 4 and 72 hours (untreated or unsuccessfully treated)
- At least two of the following:
- Unilateral location
- Pulsating quality
- Moderate to severe intensity
- Worsened by routine physical activity
- Unilateral location
Additionally, at least one of the following must be present:
- Nausea and/or vomiting
- Photophobia and phonophobia
These criteria are strict to prevent misdiagnosis, guide treatment decisions, and ensure that patients receive appropriate care.
Common Misdiagnosis Scenarios
Headaches are often misidentified, leading to ineffective treatment or unnecessary concern. Here are common scenarios and why they can be misleading:
- I Have Migraines Because My Head Hurts Badly
Severity alone does not define a migraine. A headache that is intense but produces bilateral, pressure-like pain without nausea, vomiting, or light/sound sensitivity is more likely a tension headache. Focusing solely on pain intensity can result in misdiagnosis. - My Headache Is Stress-Related, So It Must Be Tension: While stress is a frequent trigger for tension headaches, it can also provoke migraines. The presence of associated symptoms, such as nausea or sensitivity to light and sound, is a more reliable indicator than the trigger itself.
- Painkillers Help, So It’s Not a Migraine: Many people assume that if over-the-counter analgesics relieve their headache, it cannot be a migraine. In reality, early treatment can abort or shorten migraine attacks, meaning medication response is not a definitive diagnostic tool.
Can Someone Have Both?
Yes, it is common for individuals to experience both tension headaches and migraines, often at different times. Chronic tension headaches can coexist with episodic migraines, making identification more challenging.
For this reason, tracking patterns over time is essential. Noting the timing, triggers, associated symptoms, and response to treatment helps distinguish one type from the other and guides appropriate management.
When Headaches Change Pattern
Any new or unusual headache pattern warrants medical evaluation. Seek prompt care if you experience:
- A new headache after age 50
- Sudden, severe headache that peaks quickly
- Headaches that progressively worsen over time
- Neurological symptoms outside of a typical migraine aura
- Headache accompanied by fever, neck stiffness, or other systemic signs
These features may indicate a secondary cause and should not be assumed to be tension headaches or migraines until properly assessed.
Role of Headache Diaries in Diagnosis
Maintaining a headache diary is one of the most valuable tools for identifying headache type. Recording the following details helps both patients and clinicians:
- Frequency and timing of headaches
- Duration of each episode
- Triggers or precipitating factors
- Associated symptoms, such as nausea or sensitivity
- Response to medications or interventions
Careful tracking over weeks to months often provides more diagnostic clarity than imaging alone.
Imaging and Tests: When Are They Needed?
Most tension headaches and migraines do not require imaging. MRI or CT scans are typically reserved for situations with red flags:
- Abnormal neurological exam findings
- Sudden or unusual headache pattern
- Progressive worsening over time
Even if imaging is normal, a migraine diagnosis remains valid based on clinical criteria. Imaging is primarily used to rule out other underlying conditions, not to confirm primary headache disorders.
Medication Overuse Confusion
Frequent use of painkillers can obscure the true headache pattern. Medication overuse headaches often:
- Occur daily or near daily
- Improve temporarily after taking medication
- Lead to worsening of overall headache frequency over time
This can mimic chronic tension headache or chronic migraine, complicating identification. Awareness and careful monitoring of medication use are essential for accurate diagnosis.
Key Takeaways for Self-Identification
To better distinguish tension headaches from migraines, consider the following questions:
- Is the pain throbbing or pressing?
- Does physical activity worsen the headache?
- Are nausea or vomiting present?
- Are you sensitive to light or sound?
- Is the pain usually on one side of the head?
- How long does the headache last if untreated?
The overall pattern, rather than any single symptom, provides the most reliable guidance, observing trends over time, combined with knowledge of typical triggers and associated symptoms, allows for accurate self-assessment and informs when to seek professional evaluation.
Final Thoughts
Tension headaches and migraines are distinct disorders with unique patterns and impacts, confusing the two can delay effective treatment and reduce quality of life. Tension headaches are typically pressure-like, bilateral, and allow daily activities to continue, whereas migraines are neurological, often disabling, and accompanied by nausea, light or sound sensitivity, or aura.
Accurately identifying the type of headache enables better treatment decisions, prevents unnecessary medication use, and lowers the risk of headaches becoming chronic. Frequent, changing, or disabling headaches always require professional evaluation, recognizing the difference is the essential first step toward taking control of your health and finding lasting relief.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowOther Post You Might Find Helpful:
- The Complete Guide to Headache and Migraine: 7 Causes, Prevention & Treatment
- 12 Proven Ways Neck Pain Causes Headaches (and How to Stop Them)
- Headache Behind Eyes: 10 Powerful Causes and Everyday Fixes
- Dehydration Headache? 10 Proven Ways to Stop It Fast & Stay Pain-Free
- 13 Early Signs of Health Problems You Shouldn’t Ignore for Better Health
- 7 Hidden Reasons Your Brain Feels Buzzing or Overactive and How to Calm It Fast
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being