MRI vs X-Ray vs CT Scan for Pain Diagnosis: Which Imaging Should You Choose?
Pain can be confusing, frustrating, and sometimes alarming, it can appear suddenly after an injury, nag persistently without clear cause, or flare up unpredictably. Understanding exactly why it happens is critical not just for relief, but for preventing long-term damage. One of the most powerful tools doctors have to investigate pain is medical imaging.
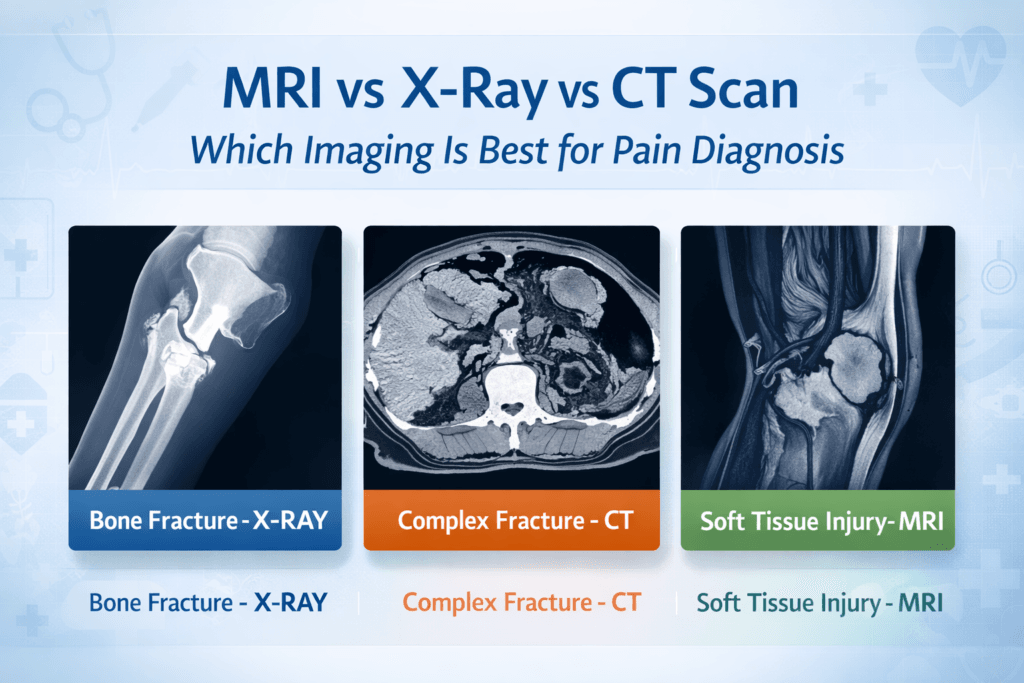
From X-rays to CT scans to MRIs, these technologies let clinicians peer inside your body and see what’s going on beneath the surface but with different options available, each suited for specific tissues and types of injuries, choosing the right imaging test isn’t always straightforward.
In this guide, we’ll break down MRI, X-ray, and CT scans, highlighting their strengths, limitations, and the situations in which each shines. By the end, you’ll understand how these imaging tools help uncover the source of pain and guide effective treatment.
Understanding Pain: Why Imaging Matters
Pain is more than just an uncomfortable sensation, it’s the body’s way of signaling that something is wrong. However, pinpointing the exact source of pain isn’t always straightforward, pain can originate from a variety of tissues, each requiring different approaches for diagnosis:
- Bone-related pain: Fractures, bone degeneration, or bone infections can cause deep, localized pain.
- Joint-related pain: Arthritis, ligament injuries, or cartilage damage often produce stiffness, swelling, or restricted movement.
- Muscle and soft tissue pain: Strains, tears, inflammation, or overuse injuries can lead to soreness, spasms, or weakness.
- Nerve-related pain: Compressed nerves, neuropathy, or nerve inflammation may cause shooting, burning, or tingling sensations.
Because pain can arise from such diverse sources, selecting the right imaging method is critical, the wrong choice can delay diagnosis, lead to unnecessary tests, or even miss the underlying problem entirely. Accurate imaging helps healthcare providers see the affected tissue clearly, guiding effective treatment and improving recovery outcomes.
X-Ray: The Oldest and Most Accessible Imaging Tool
What is an X-Ray?
X-ray imaging is one of the oldest and most widely used diagnostic tools in medicine. It uses a small, controlled dose of ionizing radiation to capture images of the body’s dense structures, primarily bones. As X-rays pass through the body, denser materials like bone absorb more radiation, appearing white on the resulting image, while softer tissues allow more radiation to pass through and appear darker. The result is a clear black-and-white image showing the structure of bones and some joint spaces.
When is X-Ray Useful?
X-rays are particularly effective for diagnosing conditions involving the bones and certain joint issues, such as:
- Bone fractures or breaks: Detects both simple and some complex fractures.
- Joint dislocations: Reveals misaligned bones in joints like the shoulder, knee, or fingers.
- Severe bone degeneration: Conditions such as advanced osteoarthritis or bone deformities.
- Bone infections (osteomyelitis): Can show changes in bone structure due to infection.
For example, if you slip and fall, landing awkwardly on your wrist, an X-ray is typically the first test performed. In many cases, it can confirm a fracture quickly and guide immediate treatment, sometimes without needing further imaging.
Strengths of X-Ray
X-rays offer several advantages that make them a cornerstone of diagnostic imaging:
- Quick and widely available: Most hospitals, urgent care centers, and even smaller clinics have X-ray machines, making it easy to access.
- Low cost: Compared with CT scans or MRIs, X-rays are highly affordable and often covered by insurance without extensive authorization.
- Effective for bone assessment: X-rays clearly reveal fractures, breaks, bone alignment, and structural changes, providing reliable information for many injuries.
Limitations of X-Ray
Despite their usefulness, X-rays have significant limitations:
- Limited soft tissue visualization: X-rays cannot clearly show muscles, ligaments, tendons, or nerves. Injuries to these tissues may remain hidden.
- Radiation exposure: Although the dose is low, repeated imaging can accumulate over time, which is a consideration for frequent scans.
- Reduced sensitivity for subtle or complex injuries: Small fractures, hairline cracks, or early-stage bone conditions may be missed. Similarly, soft tissue injuries such as ligament tears or disc problems are often invisible.
X-rays remain the first-line imaging choice for obvious bone injuries, joint dislocations, or severe degenerative changes. They are fast, accessible, and cost-effective. However, while they provide excellent structural information about bones, X-rays cannot give a complete picture of soft tissue or complex injuries. When the source of pain may involve muscles, ligaments, cartilage, or nerves, additional imaging like CT scans or MRI is often necessary.
CT Scan: Detailed Cross-Sectional Imaging
What is a CT Scan?
A CT scan uses X-ray technology in a more sophisticated way, capturing multiple images from different angles and combining them into detailed cross-sectional images of the body. This allows doctors to see bones, organs, and soft tissues in much greater detail than a standard X-ray.
When is a CT Scan Useful?
CT scans are particularly useful for:
- Complex fractures (e.g., pelvis, spine, wrist)
- Joint injuries with bone fragments
- Spinal problems (herniated discs, spinal stenosis)
- Internal bleeding or organ injury after trauma
- Tumors or cancers affecting bones and soft tissues
For instance, if someone suffers a severe car accident, a CT scan of the spine and pelvis can reveal subtle fractures and internal injuries that an X-ray would miss.
Strengths of CT Scan
- High-detail bone imaging: Excellent for detecting complex fractures.
- Soft tissue visualization: Better than X-rays for muscles, ligaments, and organs.
- Fast: Most CT scans take only a few minutes.
- Guidance for procedures: Used for biopsies or interventional radiology.
Limitations of CT Scan
- Higher radiation exposure: CT scans expose patients to significantly more radiation than X-rays.
- Limited soft tissue contrast compared to MRI: Muscle and nerve injuries are often better visualized with MRI.
- Cost: More expensive than X-rays.
CT scans are excellent for complex bone injuries, trauma evaluation, and some soft tissue problems. They provide detailed cross-sectional images but come with higher radiation exposure.
MRI: The Gold Standard for Soft Tissue
What is an MRI?
MRI uses powerful magnets and radio waves to create detailed images of the body’s internal structures. Unlike X-rays and CT scans, MRI does not use ionizing radiation, making it safer for repeated imaging. MRI is particularly sensitive to soft tissue structures, including muscles, ligaments, cartilage, and nerves.
When is MRI Useful?
MRI is the best choice for:
- Muscle and ligament injuries: Tears, strains, or sprains.
- Spinal problems: Herniated discs, nerve compression, and spinal cord lesions.
- Joint injuries: Meniscus tears, rotator cuff injuries, or cartilage damage.
- Nerve-related pain: Sciatica, neuropathies, and nerve entrapments.
- Inflammatory conditions: Arthritis, tendinitis, and other soft tissue inflammation.
For example, if a patient has persistent knee pain after an injury but X-rays show no fracture, an MRI can reveal a meniscus tear or ligament damage.
Strengths of MRI
- Superior soft tissue detail: Ligaments, cartilage, nerves, and muscles are clearly visible.
- No radiation: Safe for repeated scans and for sensitive populations (children, pregnant patients).
- Early detection: MRI can identify injuries and conditions before X-rays or CT can.
Limitations of MRI
- Time-consuming: MRI scans can take 30-60 minutes or longer.
- Cost: Significantly more expensive than X-rays and most CT scans.
- Availability: Not all clinics have MRI machines, especially in rural areas.
- Contraindications: Patients with certain metal implants or pacemakers may not be able to undergo MRI.
- Claustrophobia: The confined space of MRI machines can be uncomfortable for some.
MRI is the most sensitive imaging for soft tissue injuries and nerve-related pain. It’s ideal when X-rays and CT scans do not explain the symptoms.
Comparing MRI, CT, and X-Ray: A Quick Reference Table
Feature | X-Ray | CT Scan | MRI |
Best for | Bone fractures, dislocations | Complex fractures, trauma, some soft tissue | Soft tissue, ligaments, muscles, nerves |
Radiation exposure | Low | Moderate-high | None |
Cost | Low | Moderate-high | High |
Time | Minutes | Minutes | 30-60+ minutes |
Availability | Widely available | Widely available | Limited in some areas |
Soft tissue visualization | Poor | Moderate | Excellent |
Bone detail | Good | Excellent | Moderate |
Choosing the Right Imaging for Your Pain
Determining the most appropriate imaging method for your pain isn’t a one size fits-all decision. Several factors, type of pain, severity, patient-specific considerations, and practical constraints play a role in guiding the choice. Understanding these factors can help ensure accurate diagnosis and avoid unnecessary tests or delays.
1. Type of Pain
The type of tissue causing pain largely determines which imaging modality will be most effective:
- Bone pain after trauma: If you suspect a fracture, an X-ray is typically the first step. It can quickly confirm obvious breaks. For more complex injuries such as pelvic fractures, spinal compression, or subtle hairline fractures, a CT scan provides detailed cross-sectional images to reveal damage that X-rays may miss.
- Joint pain with suspected ligament or cartilage injury: When pain is localized to a joint, especially after twisting or repetitive strain, MRI is often the best choice. It provides high-resolution images of ligaments, tendons, cartilage, and joint capsules, allowing clinicians to pinpoint the exact source of discomfort.
- Chronic soft tissue pain: Persistent pain in muscles, tendons, or nerves especially when X-rays or CT scans appear normal often warrants an MRI. This is particularly useful for conditions like rotator cuff tears, meniscus injuries, or nerve entrapments such as sciatica.
- Acute trauma with multiple injuries: In cases of severe accidents, where multiple bones or organs may be affected, CT scans are generally preferred. They offer rapid, comprehensive views of both skeletal and soft tissue structures, helping doctors triage injuries effectively.
2. Duration and Severity
The urgency and persistence of pain also influence imaging decisions:
- Sudden, severe pain: When pain is intense and acute, imaging may need to be performed immediately to rule out fractures, dislocations, or internal injuries. X-ray or CT scans are usually preferred in these scenarios due to speed and availability.
- Chronic or unexplained pain: Pain that lingers without an obvious cause often requires more sensitive imaging. MRI can detect subtle soft tissue or nerve injuries that might otherwise go unnoticed, providing crucial information for long-term management.
3. Patient Factors
Individual circumstances can impact which imaging method is safest or most practical:
- Pregnancy: Radiation exposure should be minimized. MRI is generally considered safe during pregnancy, whereas X-rays and CT scans are used only when absolutely necessary.
- Metal implants or devices: Certain implants, pacemakers, or metal fragments may prevent MRI use due to magnetic interference. In such cases, CT or X-ray may be safer alternatives.
- Claustrophobia or anxiety: Some patients find traditional MRI machines uncomfortable due to confined spaces. Open MRI scanners or CT scans can offer a more tolerable experience without compromising diagnostic accuracy.
4. Cost and Accessibility
Practical considerations also play a significant role in imaging decisions:
- Budget constraints: X-rays are the most affordable option and often the first step. If results are inconclusive or injuries are complex, clinicians may escalate to CT or MRI.
- Availability in remote areas: While X-rays and CT scans are widely available, MRI machines may be limited to larger hospitals or urban centers. In such cases, X-ray or CT may be the only accessible option initially, with MRI used later if needed.
Choosing the right imaging for your pain involves balancing medical necessity, safety, cost, and accessibility. A clear understanding of your symptoms, combined with guidance from a healthcare professional, ensures that the right test is performed at the right time, maximizing the chances of an accurate diagnosis and effective treatment.
Risks and Considerations
While imaging is invaluable, it’s not without risks:
- Radiation exposure: Repeated X-rays and CT scans can accumulate radiation dose.
- Contrast agents: Some CT and MRI scans use dyes to enhance images, which may cause allergic reactions or kidney issues.
- Incidental findings: Imaging sometimes reveals unrelated abnormalities, causing unnecessary anxiety or procedures.
- Overuse: Not all pain requires imaging. Clinical evaluation often guides initial testing.
A careful discussion with your healthcare provider ensures imaging is appropriate and safe.
The Bottom Line: Which Imaging Is Best?
There’s no universal answer, the best imaging depends on your symptoms, suspected condition, urgency, and other individual factors.
- X-ray: Fast, cheap, excellent for bone injuries, but limited for soft tissue.
- CT scan: Highly detailed, great for complex trauma, bones, and some soft tissue, but involves higher radiation.
- MRI: Superior soft tissue and nerve imaging, no radiation, but expensive and time-consuming.
Smart Approach: Often, imaging is used in stages:
- Start simple: X-ray for obvious bone injury.
- Escalate if needed: CT for complex fractures or trauma.
- Use MRI: When soft tissue or nerve involvement is suspected or X-rays/CT don’t explain the pain.
Tips for Patients
- Know your symptoms: Detailed pain description helps doctors choose the right imaging.
- Ask about radiation: Especially if multiple scans are expected.
- Insurance and cost: Check coverage for MRI or CT before scheduling.
- Follow-up: Imaging results are one part of diagnosis; clinical correlation is critical.
- Second opinions: If results are unclear, another radiologist or specialist review can help.
Emerging Trends in Imaging
Modern technology continues to improve pain diagnosis:
- Low-dose CT: Reduces radiation while maintaining detail.
- Functional MRI (fMRI): Assesses brain activity, useful for chronic pain studies.
- Ultrasound: Increasingly used for joint and soft tissue evaluation, radiation-free and cost-effective.
- AI-assisted imaging: Enhances detection of subtle fractures or soft tissue damage.
These innovations make pain diagnosis more precise and safer.
Conclusion
Pain is never just a random sensation, it’s a signal from your body that something needs attention. Medical imaging is one of the most powerful tools for decoding that signal, helping doctors see what’s happening beneath the surface but not all imaging is the same, knowing which test to use and when, can make a significant difference in diagnosis and treatment.
- Bone injuries: X-rays are usually the first step. If fractures are complex or unclear, a CT scan provides more detail.
- Soft tissue or nerve injuries: MRI offers unmatched clarity for ligaments, muscles, cartilage, and nerves, making it the gold standard for these conditions.
- Trauma or multiple injuries: CT scans are fast, detailed, and capable of assessing both bone and some soft tissue injuries simultaneously.
The key takeaway is that imaging should support not replace clinical evaluation. Understanding the strengths, limitations, and ideal uses of X-ray, CT, and MRI empowers patients to participate in informed decisions about their care. Pain is a message, not just a symptom. Choosing the right imaging test is the first step in listening carefully, diagnosing accurately, and starting effective treatment without delay.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Blog Post:
- Essential Guide to Lower Back, Joint, and Bone Pain: Causes, Diagnosis, and Effective Treatments
- 10 Doctor-Recommended Supplements for Blood Sugar Control in Diabetes (Powerful Evidence‑Backed Guide)
- Lower Back Pain Radiates to the Leg: 7 Key Causes, Diagnosis & Treatments
- Lower Back Pain When Sitting, Standing, or Bending Forward: 7 Proven Ways to Find Relief
- Osteoarthritis vs Rheumatoid Arthritis: 7 Key Pain Patterns You Must Know
- 10 Critical Causes of Joint Pain With Swelling but No Injury (What Doctors Look For)
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


