Osteoarthritis vs Rheumatoid Arthritis: 7 Key Pain Patterns You Must Know
Arthritis isn’t just one condition, it’s a family of over a hundred joint disorders that silently chip away at mobility, comfort, and quality of life. Among these, osteoarthritis and rheumatoid arthritis are the two most common, yet they are often misunderstood and easily confused. Many people chalk their joint pain up to normal aging, but the truth is far more nuanced. The timing, location, and nature of the pain carry critical clues about what’s really happening inside your body.
Ignoring these signals can lead to years of unnecessary discomfort, worsening joint damage, and missed opportunities for early intervention. On the other hand, understanding the subtle differences between osteoarthritis and rheumatoid arthritis particularly how they manifest as pain, can empower you to seek the right treatment, protect your joints, and regain control over your daily life.
In this guide, we’ll break down the distinctions between osteoarthritis and rheumatoid arthritis with precision, exploring their symptoms, underlying mechanisms, pain patterns, progression, and management strategies. By the end, you’ll be able to read the language of your joints, recognize when something is more than just wear-and-tear, and take informed steps to protect your health before minor aches become major problems.
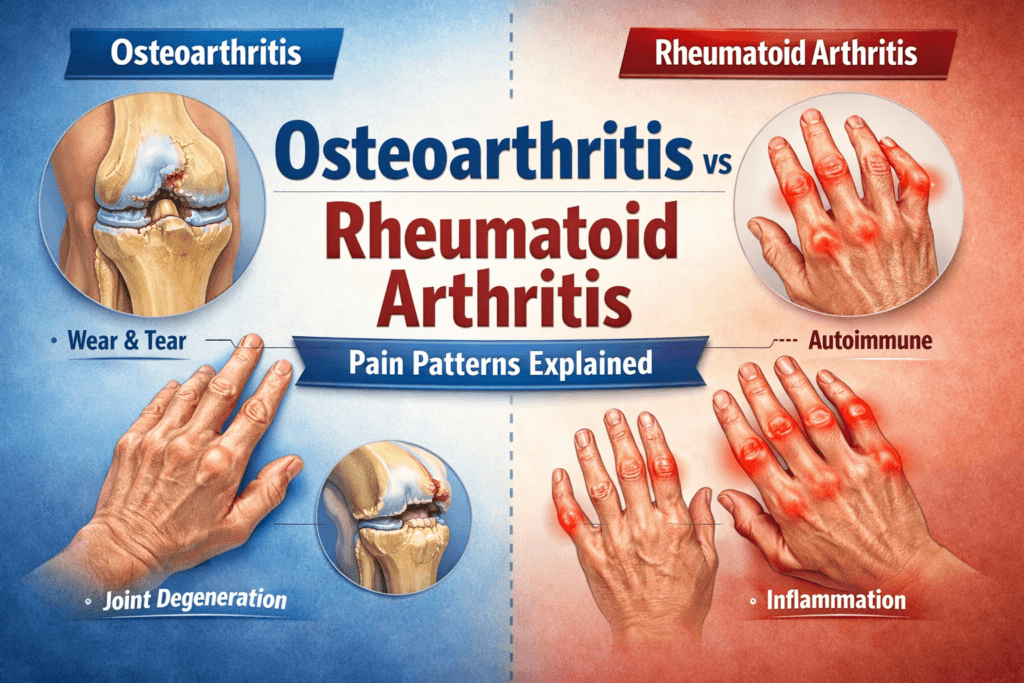
What is Osteoarthritis?
Osteoarthritis is often referred to as “wear-and-tear arthritis”, and for good reason, it develops when the cartilage, the smooth, protective layer that cushions the ends of your bones gradually breaks down. Without this cushion, bones begin to rub against each other, leading to pain, stiffness, swelling, and reduced mobility. Over time, this friction can cause structural changes in the joint, including bone spurs and deformities.
osteoarthritis primarily targets weight-bearing joints such as the knees, hips, and spine, though it can also affect the hands and fingers. Unlike inflammatory forms of arthritis, osteoarthritis is degenerative, meaning it worsens slowly over the years as cartilage deteriorates and the joint undergoes structural wear.
Key Features of osteoarthris
- Gradual onset of pain: Osteoarthritis typically develops slowly, often starting with occasional aches that worsen with activity.
- Joint stiffness: Particularly after periods of inactivity, such as sleeping or sitting for long hours.
- Reduced range of motion: The joint may feel tight or difficult to move freely.
- Occasional swelling: Mild swelling may occur, especially after prolonged activity.
- Bone spurs and deformity: In advanced stages, the joint may develop bony projections or change shape, further limiting mobility.
OA pain is usually mechanical, meaning it worsens with movement or weight-bearing activity and improves with rest. This predictable pattern helps differentiate it from inflammatory forms of arthritis.
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a chronic autoimmune disease, in which the immune system mistakenly attacks the body’s own joint tissues. Unlike osteoarthritis, rheumatoid arthritis is primarily inflammatory, targeting not only cartilage and bones but also the synovial lining of joints, the tissue that produces joint fluid. Persistent inflammation can lead to joint destruction, deformities, and even systemic complications affecting the heart, lungs, and eyes.
Rheumatoid arthritis can affect any joint, but it usually targets small joints in the hands, wrists, and feet, often in a symmetric pattern. Its onset can be rapid, and the condition often alternates between flare-ups and periods of remission.
Key Features of Rheumatoid Arthritis:
- Pain with swelling and warmth: Joints often feel tender, swollen, and warm to the touch.
- Morning stiffness: Stiffness typically lasts more than an hour, making daily tasks challenging in the morning.
- Symmetric joint involvement: The same joints on both sides of the body are usually affected.
- Systemic symptoms: Fatigue, low-grade fever, malaise, and loss of appetite are common.
- Nodules under the skin: In some cases, firm lumps (rheumatoid nodules) may develop near affected joints.
Rheumatoid arthritis pain is less predictable than osteoarthritis pain. It can occur at rest, flare suddenly, and be accompanied by systemic fatigue, making it far more than a simple joint issue.
Key Differences Between Osteoarthritis, Rheumatoid arthritis
While osteoarthritis and rheumatoid arthritis both cause joint pain, their underlying mechanisms, symptoms, and progression are markedly different. Recognizing these differences is crucial for early diagnosis and effective management.
Feature | Osteoarthritis | Rheumatoid Arthritis |
Cause | Mechanical wear-and-tear, aging, repeated joint stress | Autoimmune attack on joint tissues |
Onset | Gradual, often over years | Can be sudden or develop rapidly |
Typical Age Group | Usually over 50 | Often between 30-60 |
Joints Affected | Weight-bearing joints (knees, hips, spine), hands | Small joints (hands, wrists, feet), often symmetric |
Pain Type | Mechanical, worsens with activity | Inflammatory, worse at rest, especially mornings |
Swelling | Mild, occasional | Pronounced, persistent |
Systemic Symptoms | Rare | Common (fatigue, low-grade fever, malaise) |
Progression | Slow, degenerative | Can be rapid, destructive, and debilitating |
Understanding these distinctions is essential because treatment approaches differ significantly. Osteoarthritis, management focuses on pain relief, joint support, and slowing degeneration, while rheumatoid arthritis treatment targets the immune system to reduce inflammation, prevent joint destruction, and manage systemic effects.
By recognizing which type of arthritis you may be experiencing, you can seek appropriate medical care early, protect your joints, and take control of your long-term mobility and quality of life.
Pain Patterns in Osteoarthritis
Osteoarthritis pain is primarily mechanical, meaning it is closely tied to movement, weight-bearing, and joint use. Understanding the nuances of osteoarthritis pain can help you identify it early and tailor daily activities to reduce discomfort.
Characteristics of OsteoArthritis Pain:
- Activity-dependent: Pain usually increases during or after movement. Climbing stairs, standing for extended periods, or walking long distances can aggravate symptoms. Rest often relieves the discomfort temporarily.
- Evening worsening: As the day progresses, joints may ache due to accumulated stress and friction. This is why many people with osteoarthritis, notice their joints feel stiff or sore by nightfall.
- Localized: Pain is typically confined to the affected joint and does not radiate far, which can help differentiate it from nerve-related pain or systemic conditions.
- Tenderness: Mild tenderness may be present around joint margins, particularly after activity.
- Crepitus: A characteristic crunching or grating sensation may be felt when moving the joint, caused by the irregular surfaces of cartilage and bone rubbing together.
osteoarthritis, pain is generally predictable, most individuals can anticipate which activities will aggravate their joints and make small lifestyle adjustments to manage discomfort effectively.
Pain Patterns in Rheumatoid Arthritis
Rheumatoid arthritis pain is inflammatory, meaning it stems from the immune system attacking joint tissues rather than mechanical wear. Rheumatoid arthritis pain has a distinct pattern and often signals a more systemic process than osteoarthritis.
Characteristics of Rheumatoid arthritis Pain:
- Morning stiffness: Pain and stiffness often last more than 30-60 minutes, sometimes extending for hours. This can make simple morning tasks like buttoning a shirt or gripping a cup particularly challenging.
- Symmetric involvement: Rheumatoid arthritis usually affects the same joints on both sides of the body, such as both hands or both wrists, creating a mirror-image pattern.
- Swelling and warmth: Joints often appear swollen, red, and feel warm to the touch, reflecting active inflammation in the synovial lining.
- Persistent pain: Unlike osteoarthritis, rheumatoid arthritis pain can occur at rest, sometimes waking patients from sleep. Flare-ups may last for days or weeks.
- Fatigue-associated: Pain is often accompanied by systemic symptoms, including fatigue, low-grade fever, and malaise, signaling that the body is under an inflammatory attack.
Rheumatoid arthritis pain is less predictable than osteoarthritis pain. Flare-ups may come and go, sometimes partially resolving during remission periods, and their intensity can vary widely.
Morning Stiffness: Osteoarthritis VS Rheumatoid arthritis
Morning stiffness is one of the most reliable clues for distinguishing osteoarthritis from rheumatoid arthritis:
- Osteoarthritis: Stiffness is usually short-lived, typically less than 30 minutes, and improves with gentle movement or light activity. Many people notice a loosening up effect after walking around or stretching.
- Rheumatoid Arthritis: Stiffness is longer-lasting, often exceeding an hour, and may be accompanied by visible swelling, warmth, and tenderness. It can take several hours of gradual movement to feel relief.
Recognizing the difference in morning stiffness is crucial for early diagnosis, particularly in rheumatoid arthritis, where timely intervention can prevent long-term joint damage.
Joint Involvement Patterns
The specific joints affected and the pattern of involvement provide another key distinction between osteoarthritis and rheumatoid arthritis
- Osteoarthritis: OA typically affects weight-bearing joints like the knees, hips, and spine, as well as the finger joints, particularly the distal interphalangeal (DIP) joints. Joint involvement is often asymmetric, meaning one side may be more affected than the other. Osteoarthritis tends to be localized to a few joints rather than systemic.
- Rheumatoid Arthritis: primarily targets small joints of the hands and feet, including the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints, and usually affects them symmetrically. Larger joints such as shoulders, elbows, or knees may also become involved as the disease progresses. Rheumatoid arthritis is systemic, with the potential to affect multiple joints and organs over time.
Understanding the pattern of joint involvement not only aids in distinguishing osteoarthritis from rheumatoid arthritis but also guides doctors in selecting the appropriate diagnostic tests and treatment strategies.
Inflammation and Swelling
Inflammation is a defining feature that clearly distinguishes osteoarthritis and rheumatoid arthritis
- Osteoarthritis (OA) Swelling: Osteoarthritis is primarily a degenerative condition. Any swelling is usually mild, caused by secondary synovial irritation or joint fluid accumulation due to long-term wear-and-tear. Pain in osteoarthritis can occur even without visible swelling, making it more mechanical than inflammatory in nature.
- Rheumatoid Arthritis Swelling: Involves pronounced, persistent swelling due to immune-mediated inflammation. Joints often appear red, warm, and tender. This inflammation is not just uncomfortable, it is destructive, gradually damaging cartilage and bone over time if untreated.
In rheumatoid arthritis, pain is strongly correlated with the degree of swelling and inflammation. Recognizing persistent swelling is crucial, as it often indicates active disease that requires medical intervention.
Fatigue and Systemic Symptoms
Rheumatoid arthritis frequently affects the body beyond the joints, whereas osteoarthritis symptoms are largely joint-specific.
- Rheumatoid Arthritis Symptoms: Rheumatoid arthritis can cause chronic fatigue, low-grade fever, loss of appetite, and a general sense of malaise. Pain often feels deep and persistent, reflecting widespread inflammation rather than just joint wear. These systemic symptoms are important red flags that signal the need for immune-modulating therapies.
- Osteoarthritis Symptoms: OA is primarily localized to affected joints. Fatigue, if present, usually results from reduced mobility or the extra effort required to compensate for painful joints, rather than systemic inflammation.
Understanding these systemic differences is key to distinguishing rheumatoid arthritis from osteoarthritis, rheumatoid arthritis and ensuring appropriate treatment is initiated early.
Diagnostic Approaches
Accurate diagnosis is essential because rheumatoid arthritis can cause irreversible joint damage, while osteoarthritis management focuses on symptom control and slowing degeneration. Differentiating between these conditions requires a combination of clinical evaluation, imaging, and laboratory tests:
- Physical Exam: The doctor evaluates joint swelling, tenderness, warmth, and deformities to identify patterns suggestive of osteoarthritis OR rheumatoid arthritis
- Blood Tests: Rheumatoid arthritis often shows elevated inflammatory markers such as ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein), along with rheumatoid factor (RF) and anti-CCP antibodies. Osteoarthritis rarely exhibits systemic inflammation in blood tests.
- X-rays: In osteoarthritis, imaging typically reveals joint space narrowing, osteophytes (bone spurs), and bone remodeling. RA X-rays show joint erosion, periarticular osteopenia, and soft tissue swelling.
- Ultrasound/MRI: These imaging techniques can detect early synovial inflammation in rheumatoid arthritis, sometimes before changes appear on X-rays, allowing for prompt intervention.
Early recognition and proper diagnosis significantly improve long-term outcomes, particularly for rheumatoid arthritis, where delaying treatment can lead to permanent joint deformities.
Medical Treatments and Interventions
Treatment strategies for osteoarthritis and rheumatoid arthritis differ significantly because the underlying causes of each condition are distinct. Osteoarthritis, is primarily degenerative, while rheumatoid arthritis is autoimmune and inflammatory. Understanding these differences is essential for effective management.
Osteoarthritis Treatments:
- Pain relievers: Medications like acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) help reduce discomfort and inflammation.
- Topical analgesics: Creams or gels containing anti-inflammatory or numbing agents can provide targeted relief to affected joints.
- Physical therapy and exercise: Tailored programs improve joint mobility, strengthen surrounding muscles, and reduce pain over time.
- Corticosteroid injections: For severe flare-ups, injections can temporarily reduce inflammation and improve function.
- Joint replacement surgery: In advanced cases where cartilage loss and joint damage are extensive, procedures like knee or hip replacement can restore mobility and relieve pain.
The primary goal of osteoarthritis treatment is symptom management, improved joint function, and slowing further degeneration.
Rheumatoid Arthritis Treatments:
- Disease-modifying antirheumatic drugs (DMARDs): Medications such as methotrexate target the underlying immune response to slow disease progression.
- Biologic agents: These advanced therapies block specific immune pathways, helping reduce inflammation and prevent joint destruction.
- NSAIDs: Used to relieve pain and inflammation during flare-ups.
- Corticosteroids: Short-term use can rapidly control severe inflammation and reduce joint swelling.
- Physical and occupational therapy: Maintains joint function, flexibility, and daily living independence.
Rheumatoid arthritis treatment aims not just to control pain but to suppress the immune system, prevent joint damage, and reduce systemic complications. Early and consistent treatment can dramatically improve long-term outcomes and preserve quality of life.
When to Seek Immediate Help
Prompt medical evaluation is critical whenever arthritis symptoms worsen suddenly or become severe. Early intervention, especially for rheumatoid arthritis can prevent irreversible joint damage and improve long-term mobility. Seek medical attention if you experience:
- Sudden joint swelling, warmth, or redness: Could indicate an acute flare, infection, or rapid disease progression.
- Severe pain unrelieved by rest or medication: Persistent or escalating pain warrants professional assessment.
- Fever or systemic symptoms with joint pain: Could signal an inflammatory or infectious process requiring urgent care.
- Rapid loss of mobility or joint deformity: Immediate evaluation is necessary to prevent permanent structural damage.
Recognizing these warning signs and acting quickly ensures timely treatment, reduces the risk of long-term complications, and improves overall outcomes for both osteoarthritis and rheumatoid arthritis
The Bottom Line
Osteoarthritis and rheumatoid arthritis are both serious conditions that cause pain, but each tells a very different story. osteoarthritis reflects mechanical wear-and-tear, developing gradually over years, with pain that worsens during activity and often improves with rest. Rheumatoid arthritis, on the other hand, is inflammatory, often symmetric, and can appear suddenly. Its pain may persist at rest, be accompanied by swelling, warmth, and systemic symptoms like fatigue or low-grade fever, signaling that the body’s immune system is at work.
Recognizing these patterns is more than a medical exercise, it’s a way to listen to your body and respond before damage becomes irreversible. Neither osteoarthritis and rheumatoid arthritisis simply a normal part of aging or something you have to endure, with proper awareness, early evaluation, and the right combination of medical care and lifestyle adjustments, you can control pain, preserve mobility, and maintain a high quality of life.
Key Takeaways:
- Track the timing and triggers of your pain: Activity-related pain usually points to osteoarthritis, while prolonged morning stiffness may indicate rheumatoid arthritis.
- Pay attention to swelling, warmth, and systemic symptoms: These are often signs of RA and should not be ignored.
- Incorporate lifestyle strategies: Exercise, diet, joint protection, and rest complement medical treatment for both conditions.
- Seek early professional evaluation: A rheumatologist or orthopedic specialist can help confirm a diagnosis and start treatment before serious joint damage occurs.
Your joints are constantly sending signals about what’s happening inside your body. Understanding these messages allows you to act decisively, prevent long-term complications, and take control of your health. Pain is not your enemy, misreading or ignoring it is.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRecommended Post:
- Essential Guide to Lower Back, Joint, and Bone Pain: Causes, Diagnosis, and Effective Treatments
- Bone Pain vs Muscle Pain vs Joint Pain:7 Ways to Tell the Difference & What It Means
- 10 Proven Ways to Reduce Morning Lower Back Pain: Real Solutions That Work
- Lower Back Pain When Sitting, Standing, or Bending Forward: 7 Proven Ways to Find Relief
- Lower Back Pain Radiates to the Leg: 7 Key Causes, Diagnosis & Treatments
- 7 Hidden Causes of Chronic Lower Back Pain That Don’t Show on X-Rays
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


