13 Proven Causes of Joint Pain Without Injury
Joint pain without a clear injury can be confusing and unsettling, there’s no fall to explain it, no obvious strain or accident. You didn’t twist anything or lift incorrectly, yet your knees ache, your fingers feel stiff, your shoulders hurt, or your hips throb for no clear reason.
This type of pain is very common, especially with age, but it’s not always just getting older. In many cases, joint pain without injury points to an underlying biological process, not damage from trauma. The joint is responding to something internal rather than an external event, that distinction matters.
When joint pain is treated blindly, with painkillers, supplements, or random exercises results are often short-lived. Symptoms may ease temporarily, then return or gradually worsen. This usually happens because the real cause of the pain was never identified.
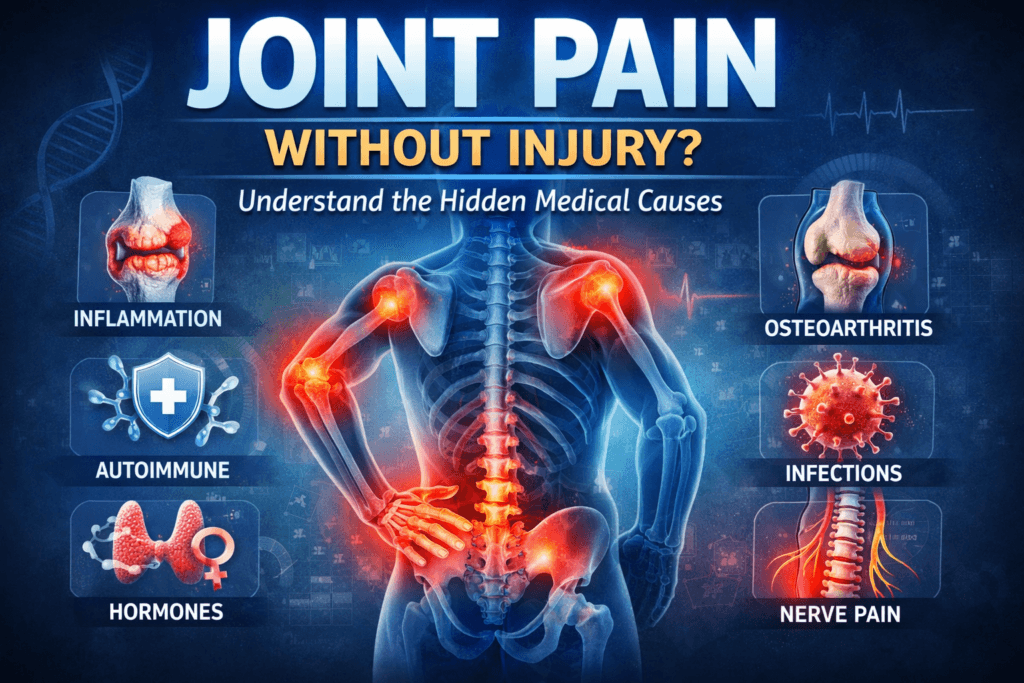
Joint pain without injury isn’t random, it follows patterns and reflects changes in inflammation, cartilage health, immune activity, hormones, metabolism, nerve signaling, or movement capacity. Until the responsible system is understood, treatment is mostly guesswork.
This article explains what’s actually happening beneath the surface clear, medically grounded reasons joints can hurt even when nothing was injured, and what that pain is really signaling. Let’s break it down properly.
Why Joint Pain Can Happen Without Injury
A joint is far more than bone meeting bone, it’s a living, dynamic system designed to move, absorb force, and adapt to stress. Each joint relies on the coordinated function of multiple tissues, including:
- Cartilage that cushions and reduces friction
- Synovial fluid that lubricates and nourishes joint surfaces
- Ligaments and tendons that provide stability and transmit force
- Muscles that control movement and protect the joint
- Nerves that regulate coordination and pain perception
- Blood vessels that supply oxygen and nutrients
- Immune cells that monitor and respond to injury or stress
Pain can originate from any of these structures, that’s why a joint can hurt even when nothing has been torn, fractured, or visibly damaged. In many cases, the pain reflects irritation, inflammation, chemical signaling, or loss of normal joint balance rather than physical injury.
Most cases of non-injury joint pain fall into six broad categories:
- Inflammatory conditions
- Degenerative joint disease
- Autoimmune disorders
- Metabolic and hormonal imbalances
- Infection and post-infection reactions
- Referred pain and nerve-related causes
Each of these produces pain through a different mechanism. Understanding which one is at play is key to effective treatment.
1. Inflammatory Joint Conditions
Inflammation is one of the most common and misunderstood causes of joint pain without injury. When inflammation is present, the immune system releases chemical messengers that irritate joint tissues. This leads to pain, stiffness, warmth, and sometimes swelling, even when no physical damage has occurred. Unlike mechanical pain, inflammatory joint pain often feels worse after rest and improves with gentle movement.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis is a chronic autoimmune disease in which the immune system mistakenly attacks the joint lining (the synovium). Over time, this inflammation can damage cartilage and bone if left untreated.
Typical features include:
- Symmetrical joint pain (both hands, both knees, both wrists)
- Morning stiffness lasting longer than 30-60 minutes
- Swelling and warmth around affected joints
- Persistent fatigue
- Gradual, progressive symptoms
RA often begins quietly. Early pain and stiffness are frequently ignored because there’s no injury to explain them. This delay in diagnosis is dangerous, untreated RA can lead to permanent joint damage and loss of function.
Psoriatic Arthritis
Psoriatic arthritis affects some people with psoriasis, but joint symptoms don’t always wait for visible skin changes. In some cases, joint pain appears years before psoriasis is diagnosed.
Common signs include:
- Joint pain and prolonged stiffness
- Swollen fingers or toes (“sausage digits”)
- Heel or foot pain
- Nail pitting or nail separation
- Periods of flare-ups followed by remission
This condition is driven by immune dysfunction, not mechanical stress. That’s why rest alone rarely resolves symptoms.
Gout (Yes, Even Without Swelling)
Gout is caused by the buildup of uric acid crystals inside a joint. While it’s famous for sudden, red, swollen attacks, not all cases look dramatic.
Some people experience:
- Deep, aching joint pain
- Pain that worsens at night
- Recurrent pain in the same joint
- Minimal or no visible swelling
The big toe is the classic site, but gout commonly affects the ankles, knees, wrists, and fingers without proper management, attacks tend to become more frequent over time.
2. Degenerative Joint Disease (Osteoarthritis)
Osteoarthritis (OA) is the most common cause of joint pain without injury. It’s often described as “wear and tear,” but that explanation oversimplifies what’s really happening.
OA is a complex condition involving:
- Gradual cartilage thinning
- Reduced joint lubrication
- Structural changes in bone
- Weakness of surrounding muscles
- Increased sensitivity of the nervous system
Why Osteoarthritis Pain Appears Without Injury
Osteoarthritis develops slowly. There’s rarely a single moment when something “breaks.” Instead:
- Cartilage loss occurs over years
- Small, repeated stresses accumulate
- Muscle imbalances increase joint load
- Movement patterns become less efficient
- Pain sensitivity increases
The result is pain that seems to come out of nowhere, even though the process has been building quietly in the background.
Joints most commonly affected include:
- Knees
- Hips
- Hands
- Spine
- Shoulders
OA pain often worsens with activity, but stiffness after rest, especially in the morning or after sitting is also common.
One crucial point, imaging doesn’t equal pain, X-rays and MRIs don’t always match symptoms. Someone with mild arthritis may have severe pain, while another person with advanced joint changes may function with very little discomfort. Pain is influenced by more than just structural damage.
3. Autoimmune and Systemic Conditions
Not all joint pain originates in the joint itself. In autoimmune and systemic diseases, pain is part of a whole-body immune response, not localized joint damage. The immune system becomes overactive or misdirected, producing inflammation that affects joints along with other organs and tissues.
Lupus (Systemic Lupus Erythematosus, SLE)
Systemic lupus erythematosus is a complex autoimmune disease that can cause significant joint pain without permanently damaging the joints. The pain comes from inflammation in the joint lining rather than structural breakdown.
Common symptoms include:
- Migratory joint pain that moves from one joint to another
- Persistent fatigue
- Skin rashes, often across the face
- Sensitivity to sunlight
- Mouth or nasal ulcers
One hallmark of lupus-related joint pain is variability. Symptoms may flare suddenly, improve, then return without warning. Because imaging often looks normal, lupus-related joint pain is sometimes dismissed, leading to delays in diagnosis.
Ankylosing Spondylitis
Ankylosing spondylitis is a chronic inflammatory condition that primarily affects the spine and pelvis but can also involve the hips, shoulders, and other peripheral joints.
Key features include:
- Significant morning stiffness
- Pain that improves with movement rather than rest
- Night pain that disrupts sleep
- Gradual loss of spinal flexibility
Unlike mechanical back pain, ankylosing spondylitis often begins in young adults. It is frequently misdiagnosed as muscle strain or poor posture, allowing inflammation to progress unchecked for years.
4. Metabolic and Hormonal Causes
Joint pain is not always caused by structural joint disease. Metabolic and hormonal imbalances can alter tissue quality, circulation, and inflammationleading to pain that feels joint-related even when the joint itself appears normal.
Diabetes-Related Joint Pain
Diabetes affects far more than blood sugar. Chronically elevated glucose alters connective tissue, impairs blood flow, and increases systemic inflammation.
Common joint-related manifestations include:
- Stiffness in the hands and shoulders
- Frozen shoulder
- Carpal tunnel syndrome
- Widespread joint discomfort
High blood sugar promotes collagen stiffening and reduces tissue elasticity, which limits joint mobility and increases pain. These changes often develop gradually, making the connection to diabetes easy to miss.
Thyroid Disorders
Both hypothyroidism and hyperthyroidism can cause joint and muscle pain without visible joint damage.
Clues pointing toward a thyroid cause include:
- Ongoing fatigue
- Unexplained weight changes
- Cold or heat intolerance
- Hair thinning or hair loss
- Joint stiffness without significant swelling
Thyroid-related joint pain often improves significantly once hormone levels are properly regulated, highlighting the importance of identifying the root cause rather than treating pain alone.
Hormonal Changes (Especially Menopause)
Estrogen plays a protective role in joint and connective tissue health. As estrogen levels decline particularly during menopause, joint pain becomes more common.
During this transition:
- Inflammatory activity increases
- Cartilage hydration decreases
- Pain sensitivity rises
This combination explains why many women develop new or worsening joint pain in their 40s and 50s, even without injury or arthritis visible on imaging.
5. Infections and Post-Infectious Joint Pain
Joint pain can persist after an infection has resolved. In these cases, the immune system remains activated, continuing to irritate joint tissues.
Viral Arthritis
Several viral infections can trigger temporary joint inflammation, including:
- Parvovirus
- Hepatitis
- Chikungunya
- COVID-19
Joint pain may last weeks or even months after the initial illness, despite no ongoing infection. While symptoms often resolve over time, the pain can be intense and disabling during recovery.
Reactive Arthritis
Reactive arthritis occurs after certain bacterial infections, typically involving the gastrointestinal or genitourinary system. The joints themselves are not infected; instead, the immune system continues to react even after the infection has cleared.
Pain, stiffness, and swelling appear because immune activity remains elevated—targeting joint tissues as collateral damage.
6. Referred Pain and Nerve-Related Causes
Sometimes, the painful joint is not the source of the problem at all.
Nerve Compression
Nerves originating from the spine supply sensation and control to joints. When these nerves are compressed or irritated, they can produce pain that feels like it’s coming from the joint.
Common examples include:
- Hip pain originating from lumbar disc issues
- Shoulder pain caused by cervical spine problems
- Knee pain referred from the lower back
In these cases:
- Joint imaging often appears normal
- Pain may worsen with specific postures or movements
- Neurological symptoms such as tingling or weakness may be subtle or intermittent
Myofascial Pain
Muscles can also refer pain to nearby joints when they become tight, overworked, or dysfunctional.
This is especially common with:
- Prolonged desk work
- Poor posture
- Physical deconditioning
- Chronic stress and muscle tension
Myofascial pain can closely mimic joint disease, leading people to focus on the joint while the true source of pain remains untreated.
Why Painkillers Often Don’t Fix Joint Pain
Painkillers can be useful in the short term, but they are rarely a complete solution for joint pain without injury. They work by dulling pain signals or reducing surface-level inflammation, not by correcting the process that caused the pain in the first place.
Pain medications do not:
- Reduce autoimmune activity
- Restore or protect cartilage
- Improve joint stability or muscle support
- Correct metabolic or hormonal dysfunction
- Retrain poor movement patterns
As a result, symptoms often return as soon as the medication wears off. In some cases, painkillers create a false sense of improvement, allowing people to push through activities that further stress an already vulnerable joint. Over-reliance on medication can also delay proper diagnosis. When pain is constantly masked, underlying inflammatory or autoimmune conditions may progress silently, leading to worse long-term outcomes and more difficult treatment later on.
When to Take Joint Pain Seriously
Joint pain without injury should never be ignored when certain warning signs are present. These features suggest an underlying medical cause that requires evaluation,not guesswork or self-treatment.
Take joint pain seriously if you notice:
- Pain persisting longer than 4-6 weeks
- Morning stiffness lasting more than 30 minutes
- Visible swelling, warmth, or redness
- Symmetrical joint involvement (both sides of the body)
- Fatigue or other systemic symptoms
- Pain that wakes you at night
- Gradually worsening or spreading pain
Early evaluation makes a real difference. Inflammatory and autoimmune joint conditions respond far better when identified and treated early, before permanent damage or chronic pain patterns develop.
How Joint Pain Is Properly Diagnosed
Accurate diagnosis is not based on a single test or scan. It requires understanding patterns, how symptoms behave over time, how they respond to movement or rest, and how they fit into the broader health picture.
A proper assessment may include:
- A detailed medical and symptom history
- A focused physical examination
- Blood tests to check inflammatory and autoimmune markers
- Imaging such as X-rays, ultrasound, or MRI when appropriate
- Functional movement assessment to evaluate strength, control, and joint loading
Imaging alone rarely tells the full story. Many people have abnormal scans without pain and severe pain with minimal findings. Diagnosis comes from connecting the dots, not chasing isolated results.
What Actually Helps Joint Pain Without Injury
Effective management depends on the underlying cause, but successful treatment usually addresses more than just pain.
Key components often include:
- Treating the source of inflammation or immune dysfunction
- Improving joint strength, support, and stability
- Restoring efficient, pain-free movement patterns
- Addressing metabolic and hormonal health when relevant
- Calming nervous system sensitivity that amplifies pain
- Avoiding unnecessary or excessive joint overload
There is no single fix that works for everyone. But there is a correct approach for each cause and when treatment targets the right mechanism, long-term improvement becomes far more achievable.
The Bottom Line
Joint pain without injury is not random, imaginary, or simply the price of getting older. It’s not something to brush off, power through, or permanently silence with painkillers. It is a signal and signals exist for a reason.
Sometimes that signal comes from inflammation, quietly irritating joint tissues long before visible damage appears. Sometimes it’s degeneration, building slowly over years rather than arriving with a single injury.
Sometimes it’s immune dysfunction, where the body mistakenly targets its own joints.
Sometimes it’s a hormonal or metabolic imbalance, altering tissue quality and pain sensitivity.
Sometimes the joint itself isn’t the problem at all, nerves, muscles, or movement patterns are the real source of pain.
What matters most is this, joint pain without injury always has a cause, even if it isn’t obvious at first. Treating symptoms without understanding that cause leads to temporary relief at best and prolonged frustration at worst.
Long-term improvement doesn’t come from guessing. It comes from identifying the mechanism behind the pain and addressing it directly. When the right system is treated whether immune, metabolic, mechanical, or neurological, joints often improve far more than people expect.
Pain is not the enemy, It’s information. Ignoring the message is what allows small, manageable problems to become chronic ones. Understanding it is what opens the door to real, lasting relief.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Blog Post:
- Essential Guide to Lower Back, Joint, and Bone Pain: Causes, Diagnosis, and Effective Treatments
- 15 Proven Natural Ways to Improve Joint Stiffness Without Medication
- 7 Surprising Causes of Joints Cracking Loudly and How to Stop It
- 7 Alarming Signs of Vitamin D Deficiency Fatigue and Joint Pain
- 10 Proven Ways to Reduce Morning Lower Back Pain: Real Solutions That Work
- Lower Back Pain When Sitting, Standing, or Bending Forward: 7 Proven Ways to Find Relief
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


