Lower Back Pain Radiates to the Leg: 7 Key Causes, Diagnosis & Treatments
Lower back pain that radiates into the leg is one of the most commonly misdiagnosed pain patterns in medicine, many people are told they have sciatica without explanation, while others hear nerve compression”and assume something is seriously wrong with their spine, both interpretations are usually incomplete.
Radiating leg pain follows specific nerve pathways and occurs for predictable mechanical and neurological reasons. It is not random, and it does not automatically mean spinal damage or the need for surgery. When the underlying mechanism is understood, diagnosis becomes precise and treatment becomes targeted instead of guesswork.
This article explains:
- What sciatica actually means and what it does not
- How nerve compression differs from sciatica
- Why pain travels from the lower back into the leg
- How to identify which structure is involved
- Evidence-based treatment options
- The difference between mechanical and neurological pain
- Red flags that require urgent medical evaluation
No myths, no vague reassurance. Just clear anatomy, clinical reasoning, and practical insight to help you understand the pain and choose the right next step.
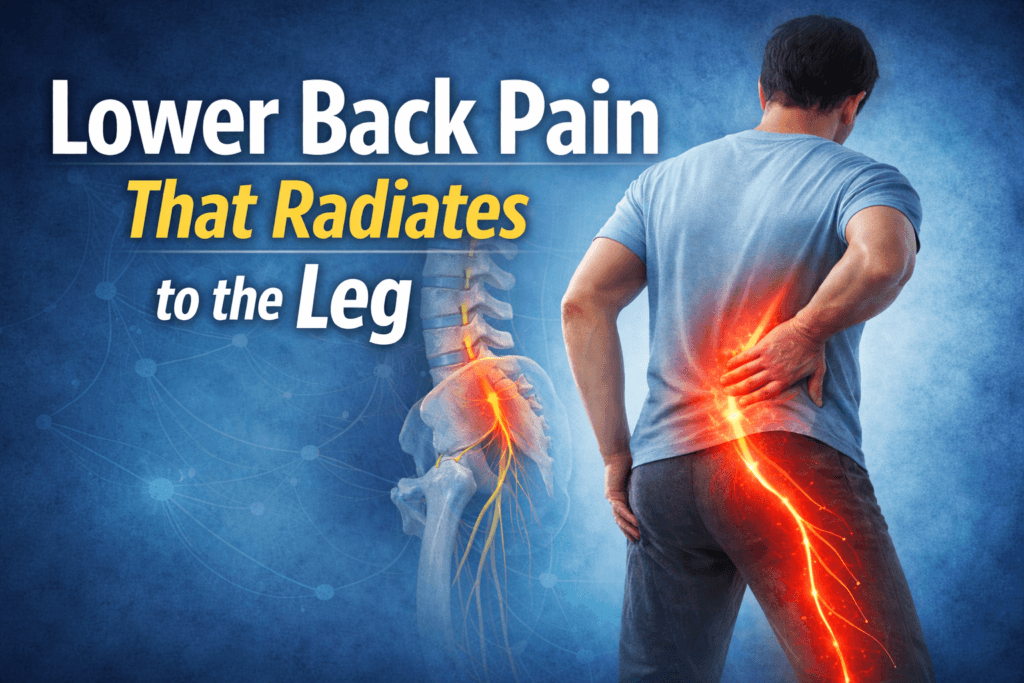
Why Lower Back Pain Radiates to the Leg
Radiating leg pain is not random, it follows the anatomy of the nervous system.
The nerves that control sensation and movement in the legs originate in the lumbar spine (L1-L5) and sacral spine (S1-S3). These individual nerve roots merge to form the sciatic nerve,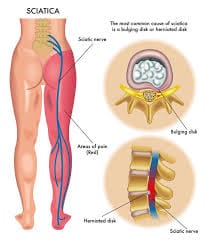 the largest and longest nerve in the human body.
the largest and longest nerve in the human body.
When any part of this system becomes irritated, compressed, inflamed, or sensitized, pain can travel along the nerve’s pathway. As a result, discomfort may:
- Start in the lower back
- Move through the buttock
- Travel down the back, side, or front of the leg
- Reach the calf, ankle, or foot
This traveling pain pattern is known as radicular pain.
Crucially, radicular pain describes how pain behaves, not what is causing it, it is a symptom pattern, not a diagnosis.
What Is Sciatica?
Sciatica is not a disease and not a structural diagnosis, it is a specific symptom pattern.
Clinically, sciatica refers to:
Pain caused by irritation or compression of the sciatic nerve or its contributing nerve roots, most commonly L4-S3.
True sciatica has recognizable features:
- Pain follows a clear nerve distribution
- It usually affects one leg
- The pain is often described as sharp, electric, burning, or shooting
- It may be accompanied by:
- Numbness
- Tingling
- Muscle weakness
- Changes in reflexes
- Numbness
Sciatica tells you which nerve pathway is involved, but it does not explain why that nerve is irritated.
What Is Nerve Compression?
Nerve compression describes a mechanical process, not a symptom.
It means: A nerve is physically narrowed, pressured, or restricted by surrounding structures.
Compression can occur in several locations, including:
- Intervertebral discs
- Vertebrae
- Facet joints
- Ligaments
- Muscles
- The spinal canal
- The foraminal openings where nerves exit the spine
Nerve compression may cause pain, numbness, weakness or sometimes no symptoms at all. The presence of compression on imaging does not automatically mean it is responsible for the pain.
Sciatica can result from nerve compression, but not all nerve compression produces classic sciatica.
Sciatica vs Nerve Compression: The Critical Difference
Feature | Sciatica | Nerve Compression |
What it is | A symptom pattern | A physical mechanism |
Refers to | Sciatic nerve involvement | Any nerve being compressed |
Always painful | Yes | Not always |
Always radiates | Yes | Sometimes |
Requires disc herniation | No | No |
Can occur without back pain | Yes | Yes |
Sciatica describes how pain behaves, nerve compression describes what is happening structurally. They often overlap, but they are not interchangeable terms. Confusing the two leads to vague diagnoses, unnecessary fear, and poorly targeted treatment. Understanding the difference is the foundation for choosing the right investigation and the right intervention.
Common Causes of Radiating Leg Pain
Radiating leg pain can arise from multiple causes, some originating in the spine, others outside it. Understanding the underlying mechanism is essential for accurate diagnosis and treatment.
1. Lumbar Disc Herniation
A disc herniation occurs when the soft inner part of a spinal disc (nucleus pulposus) pushes outward and irritates a nearby nerve root.
Important clarifications:
- Pain is often caused by chemical inflammation, not just mechanical pressure.
- Small herniations can produce severe pain, while large herniations can be painless.
Typical symptoms:
- Sharp leg pain that may be worse than back pain
- Pain worsens with sitting or bending forward
- Coughing, sneezing, or straining can intensify symptoms
- Numbness, tingling, or leg weakness may occur
2. Lumbar Spinal Stenosis
Spinal stenosis is the narrowing of the spinal canal, which can compress nerve roots. It is more common in adults over 50.
Key features:
- Leg pain worsens with walking or standing
- Pain improves with sitting or bending forward
- Often affects both legs
- Pain may feel like heaviness or fatigue rather than sharp pain
While this is a form of nerve compression, it is not classic sciatica.
3. Foraminal Stenosis
In foraminal stenosis, nerves are compressed as they exit the spine rather than in the central canal.
Symptoms:
- Pain usually affects one side
- Pain worsens with spinal extension
- May be position-dependent
- Can mimic sciatica, making accurate diagnosis important
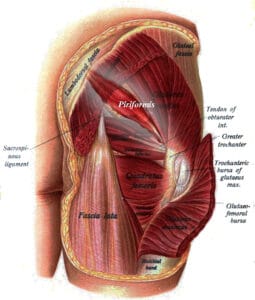
4. Piriformis Syndrome (Non-Spinal Cause)
The piriformis muscle, located deep in the buttock, can irritate the sciatic nerve outside the spine.
Features:
- Prominent buttock pain
- Pain worsens with prolonged sitting
- Lower back pain may be minimal or absent
- Spine imaging may appear normal
This represents true sciatic nerve irritation without spinal compression.
5. Spondylolisthesis
Spondylolisthesis occurs when one vertebra slips forward relative to another, potentially narrowing nerve pathways and altering spinal mechanics.
Consequences:
- Can cause progressive nerve symptoms
- Pain often worsens with standing or spinal extension
6. Degenerative Disc Disease
Despite the alarming name, degenerative disc disease is usually an age-related structural change, not an active disease.
Symptoms occur when:
- Disc height loss narrows nerve space
- Inflammation sensitizes nerve roots
- Movement patterns overload specific spinal segments
How to Tell Which Nerve Is Involved
The location of leg pain provides strong clues about which nerve root is affected:
Pain Location | Likely Nerve Root |
Front of thigh | L2-L3 |
Knee and inner leg | L3-L4 |
Outer leg to big toe | L5 |
Back of leg to heel | S1 |
Outer foot | S1-S2 |
True sciatica most often involves the L5 or S1 nerve roots, which explains why pain commonly travels down the back or outer side of the leg.
Mechanical Pain vs Neurological Pain
Not all leg pain originates from nerves. Understanding the difference between mechanical pain and neurological pain is critical because treatment strategies differ.
Mechanical Pain
Mechanical pain arises from muscles, joints, ligaments, or discs rather than the nerves themselves. Key characteristics include:
- Dull, aching, or stiff sensation
- Changes with posture, pain may worsen when standing, sitting, or bending in certain positions
- Improves with rest or gentle movement
- Localized to the lower back or a specific region of the leg
Neurological Pain
Neurological pain occurs when nerves are irritated or compressed, producing distinct patterns:
- Sharp, electric, burning, or shooting pain
- Radiates along a clear nerve path, often down the leg
- May be accompanied by numbness, tingling, or muscle weakness
- Often worse at night, especially when nerve irritation increases in certain positions
Why this distinction matters:
Treating mechanical pain focuses on restoring mobility and strength, while neurological pain may require targeted nerve-focused interventions, misdiagnosis can delay recovery and lead to unnecessary treatments.
Imaging: When MRI Helps (And When It Doesn’t)
MRI can be a useful tool, but only when interpreted in context with clinical symptoms.
Key facts about MRI:
- Many people have disc herniations or degenerative changes without any pain
- Imaging abnormalities increase with age, even in pain-free individuals
- An MRI alone cannot diagnose the cause of pain
MRI is most useful when:
- Pain persists beyond 6-8 weeks despite conservative care
- There is progressive weakness or neurological deficits
- Surgery is being considered
- Red flags are present, indicating potential serious pathology
Rule of thumb: Treat the patient, not the scan. Clinical evaluation and symptom patterns are far more informative than imaging alone.
Evidence-Based Treatment Options
1. Activity Modification
Prolonged rest can slow recovery and increase stiffness, instead:
- Avoid positions that worsen pain
- Maintain gentle movement to keep muscles and joints active
- Gradually reintroduce loading to rebuild strength and endurance
2. Physical Therapy
Effective rehabilitation focuses on:
- Spinal stability and core strength
- Hip and lower extremity mobility
- Nerve glide techniques to reduce irritation
- Load tolerance training to improve functional capacity
Random or generic exercises are rarely effective for radiating leg pain.
3. Anti-Inflammatory Strategies
Short-term symptom relief may include:
- NSAIDs under medical supervision
- Heat or cold therapy depending on comfort
- Activity pacing to avoid aggravating structures
These strategies manage symptoms, but do not address the underlying cause.
4. Epidural Steroid Injections
Steroid injections may help when:
- Inflammation is a dominant contributor to nerve irritation
- Pain limits participation in rehabilitation
- Short-term relief allows return to functional activity
They do not fix discs and are intended to facilitate recovery, not replace conservative care.
5. Surgery
Surgical intervention is considered only when:
- There are progressive neurological deficits
- Severe leg weakness develops
- Pain remains disabling despite conservative therapy
Most cases of radiating leg pain do not require surgery, conservative management remains the first-line approach.
Why Chronic Radiating Pain Persists
Chronic leg pain is rarely caused by ongoing structural damage. Contributing factors often include:
- Nervous system sensitization, where the nerves become overly responsive
- Fear-avoidance behaviors, limiting movement and increasing stiffness
- Deconditioning, leading to weaker muscles and reduced spinal support
- Poor load management, placing stress on nerves and joints
The nervous system learns pain, but it can also unlearn it with the right interventions.
Red Flags That Require Immediate Medical Evaluation
Seek urgent care if you experience:
- Loss of bladder or bowel control
- Saddle numbness (numbness around the groin or inner thighs)
- Progressive leg weakness
- Unexplained weight loss
- Fever with back pain
- History of cancer with new or worsening pain
These cases are rare but indicate potentially serious underlying conditions that require prompt evaluation.
The Bottom Line
Lower back pain that radiates into the leg is common, often misunderstood, and usually manageable. It is not always sciatica, and it is not inherently dangerous.
Understanding the distinction between sciatica and nerve compression is crucial:
- Sciatica describes a pain pattern, how symptoms travel along the nerve.
- Nerve compression describes a mechanical process, what is physically affecting the nerve.
Recognizing this difference empowers you to:
- Achieve a more accurate diagnosis rather than relying on vague labels
- Follow targeted treatments that address the true cause of pain
- Recover more efficiently, with less unnecessary fear or hesitation
- Make informed decisions about interventions, whether conservative or medical
Most cases of radiating leg pain improve with time, consistent movement, and structured rehabilitation. Rarely does it indicate irreversible damage. Back pain is less about structural failure and more about capacity, the ability of muscles, joints, and nerves to handle everyday loads.
The encouraging reality is that capacity can be rebuilt with the right guidance, movement, and understanding, you can reduce pain, restore function, and regain confidence in your body. Radiating leg pain is not a sentence, it’s a signal that, with the right approach, recovery is possible.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowMust Read:
- Essential Guide to Lower Back, Joint, and Bone Pain: Causes, Diagnosis, and Effective Treatments
- 7 Hidden Causes of Chronic Lower Back Pain That Don’t Show on X-Rays
- 7 Bone Density Boosters That Really Work, Supercharge Your Bone Health
- 15 Proven Natural Ways to Improve Joint Stiffness Without Medication
- 7 Alarming Signs of Vitamin D Deficiency Fatigue and Joint Pain
- Diabetic Neuropathy Explained: 12 Brutal Reasons High Sugar Destroys Nerves
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being