⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
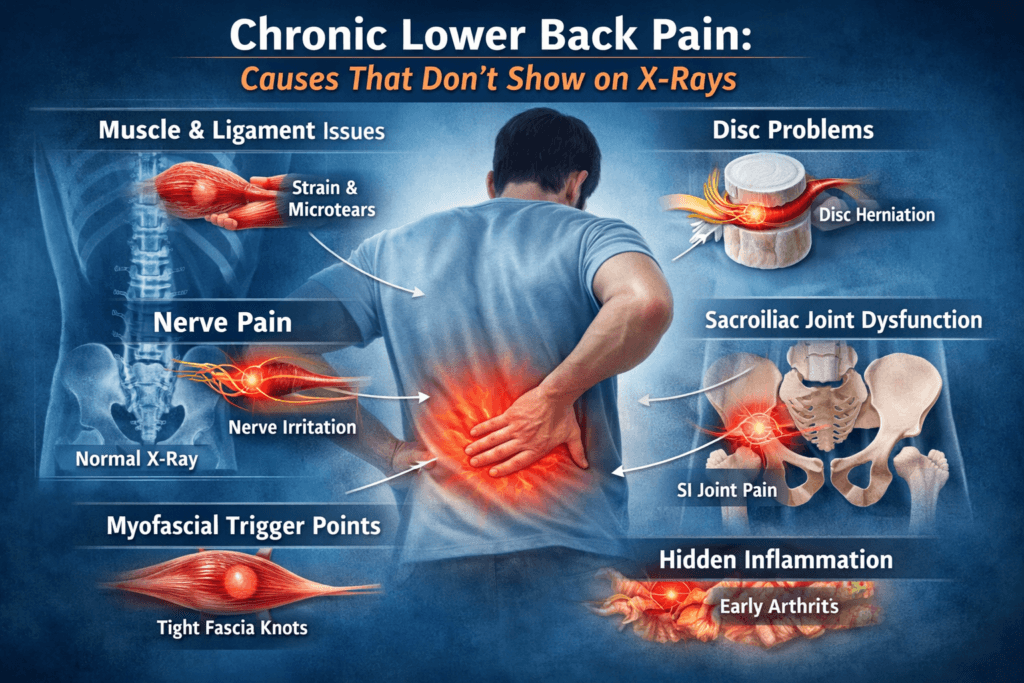
7 Hidden Causes of Chronic Lower Back Pain That Don’t Show on X-Rays
Lower back pain is one of the most common medical complaints worldwide, millions of people wake up each day with stiffness, soreness, or debilitating discomfort that can limit their work, hobbies, and daily life. For many, X-rays are often the first imaging tool ordered by physicians, yet time and again, patients are told your X-rays look normal, despite persistent pain.
This disconnect between pain experience and imaging findings can be frustrating and confusing. Chronic lower back pain often originates from causes that X-rays simply cannot detect. Understanding these invisible triggers is key to effective management and long-term relief. In this article, we explore why lower back pain can persist even with normal imaging, the underlying mechanisms, and practical strategies to address it.
The Limitations of X-Rays
X-rays are widely available, inexpensive, and excellent at showing bones. They can detect fractures, dislocations, bone spurs, and advanced degenerative changes. However, they have significant limitations when it comes to soft tissues, nerves, and subtle functional changes.
Specifically, X-rays cannot reliably show:
- Muscle or ligament strain
- Early disc degeneration
- Inflammatory changes
- Nerve irritation
- Fascia or connective tissue dysfunction
As a result, a normal X-ray does not guarantee the absence of underlying pathology. Pain is a complex signal processed by your nervous system, not just a reflection of visible structural damage.
1. Muscle and Ligament Dysfunction
One of the most common yet invisible causes of chronic lower back pain is dysfunction in the muscles and ligaments that support the spine. Muscles like the erector spinae, multifidus, and psoas are critical for maintaining spinal stability, supporting posture, and enabling movement. When these muscles are weak, imbalanced, or overworked, even normal daily activities can trigger persistent pain.
Muscle-related pain can develop from:
- Overuse or repetitive strain: Repeating the same movements over time can fatigue muscles, leading to small microtears and inflammation.
- Weakness and poor conditioning: A weak core and back muscles fail to provide adequate spinal support, transferring more stress to ligaments and discs.
- Muscle imbalances: When some muscles overcompensate for weaker ones, uneven forces can irritate soft tissue and joints.
- Microtears in muscle fibers: Tiny injuries in muscles do not show up on X-rays, yet they can create chronic discomfort and stiffness.
Ligaments, the fibrous bands that connect bones, provide passive stability to the spine. Chronic stress, trauma, or poor posture can cause ligamentous microdamage, which may inflame surrounding tissues, leading to persistent pain, stiffness, and a feeling of instability.
Chronic lower back pain can persist even when bones appear intact on X-ray because soft tissues like muscles and ligaments can be damaged or dysfunctional without leaving visible traces.
2. Disc Degeneration and Herniation
Intervertebral discs act as shock absorbers between vertebrae, allowing smooth movement and load distribution. Over time, or following injury, discs can degenerate or develop herniations. Early-stage disc degeneration or subtle bulges often cannot be detected on X-rays, which only capture bone density and alignment.
MRI is the gold standard for detecting disc problems, revealing:
- Mild disc dehydration: Loss of water content in discs can reduce cushioning and flexibility.
- Small bulges or protrusions: Even minor bulges can irritate nearby nerves or alter spinal mechanics.
- Annular tears: Tiny tears in the disc wall that can trigger inflammation and localized pain.
Interestingly, research shows that some individuals with disc degeneration on MRI experience no pain, while others with completely normal imaging suffer severe discomfort. This highlights the disconnect between structural changes and the perception of pain. Pain is not always proportional to what appears on imaging.
Bottom line, discs can degenerate or become irritated long before X-rays reveal anything abnormal, making MRI or CT crucial when chronic pain persists.
3. Nerve-Related Pain: The Invisible Culprit
The nervous system plays a central role in chronic lower back pain. Irritation, compression, or inflammation of spinal nerves can create radiating pain, tingling, numbness, or burning sensations, often extending down the legs or buttocks.
Common nerve-related conditions include:
- Sciatica: Compression or irritation of the sciatic nerve causing pain that travels from the lower back into the legs.
- Spinal stenosis: Narrowing of the spinal canal that puts pressure on nerve roots.
- Nerve root inflammation: Often due to minor disc bulges or joint dysfunction, irritating nerves without visible bone changes.
Because nerves are not visible on X-rays, these conditions often go undetected until advanced imaging (MRI or CT) is performed.
Another critical factor is central sensitization, a condition in which the nervous system becomes hyperactive and overly responsive to stimuli. In this state, even minor triggers can provoke intense pain, creating a self-perpetuating cycle of nerve overactivity, muscular tension, and persistent discomfort.
Chronic lower back pain can be nerve-driven and invisible on X-ray, requiring a combination of clinical evaluation and advanced imaging for accurate diagnosis.
4. Sacroiliac Joint Dysfunction
The sacroiliac (SI) joint, located at the junction of the lower spine and pelvis, is often an overlooked source of lower back pain. Dysfunction or inflammation in this joint may cause pain and stiffness, yet X-rays rarely reveal early-stage issues unless arthritis is advanced.
Common symptoms of SI joint dysfunction include:
- Deep lower back or buttock pain
- Pain when rising from a chair or standing after sitting
- Discomfort when walking, climbing stairs, or carrying loads
Diagnosing SI joint problems typically relies on physical examination and specialized provocation tests, sometimes combined with diagnostic injections. Imaging alone is usually insufficient to confirm the condition, particularly in the early stages.
The SI joint can be a hidden source of chronic pain, reinforcing the idea that normal X-ray results do not rule out significant spinal dysfunction.
5. Myofascial Pain Syndrome
The fascia is a dense network of connective tissue that surrounds and supports muscles, nerves, and organs throughout the body. When fascia becomes tight, restricted, or develops trigger points (knots), it can create myofascial pain syndrome, a common, often overlooked cause of chronic lower back discomfort.
Typical characteristics include:
- Localized pain that may radiate: Pain often spreads along a predictable pattern, following nerve and muscle pathways.
- Muscle stiffness: Tight fascia restricts movement and creates a sensation of heaviness or tension in the lower back.
- Tender points: Pressing on specific spots can reproduce pain, confirming trigger points.
Standard X-rays cannot visualize fascia, making this condition completely invisible to routine imaging. Effective management usually involves manual therapy, targeted stretching, dry needling, and exercises that release tension, restore mobility, and strengthen surrounding muscles.
6. Inflammatory Causes: Early Arthritis and Autoimmune Disorders
Early stages of inflammatory conditions like ankylosing spondylitis or other autoimmune-related arthritis may not show any noticeable changes on X-rays. Yet, they can cause persistent, deep-seated lower back pain that gradually worsens.
Symptoms often include:
- Deep, aching lower back pain
- Morning stiffness that improves with movement
- Fatigue and general malaise
Detecting inflammation early is critical, as untreated autoimmune conditions can silently progress and eventually cause structural damage. Diagnosis often relies on a combination of blood tests, MRI, and thorough clinical evaluation, rather than X-rays alone.
Early inflammatory pain can be invisible on conventional imaging but requires timely recognition to prevent long-term disability.
7. Psychological and Central Nervous System Factors
Chronic lower back pain is rarely purely structural. The brain and nervous system play a major role in pain perception. Stress, anxiety, depression, and past trauma can amplify pain signals, making discomfort feel more intense or persistent.
Important considerations:
- Pain is not imaginary, even if structural damage is absent on X-rays.
- Psychological stress can increase muscle tension, reduce blood flow, and slow healing.
- Mind-body interventions such as cognitive-behavioral therapy (CBT), mindfulness, and stress management can significantly improve outcomes.
This highlights the mind-body connection in chronic lower back pain, addressing psychological factors is as important as treating physical issues.
8. Poor Posture and Biomechanics
Subtle postural deviations and biomechanical imbalances often generate chronic lower back pain without producing any visible changes on X-ray. Common contributors include:
- Pelvic tilt or rotation that disrupts spinal alignment
- Unequal leg length, which shifts weight distribution and stresses the spine
- Weak core muscles, reducing spinal support
- Improper lifting or movement mechanics, causing repeated microtrauma
Over time, these minor imbalances can create cumulative damage in muscles, ligaments, and joints. Correcting posture, strengthening the core, and engaging in functional movement training are often more effective than relying solely on imaging to identify pain sources.
9. Lifestyle Factors That Exacerbate Pain
Lifestyle and systemic factors can worsen chronic lower back pain, and many are undetectable on X-rays:
- Sedentary behavior: Weakens core and back muscles, reducing spinal support.
- Obesity: Increases mechanical stress on the lower back.
- Poor sleep quality: Impairs healing and amplifies pain perception.
- Smoking: Reduces blood flow to spinal tissues, slowing repair and increasing degenerative risk.
- Nutritional deficiencies: Low levels of vitamin D, calcium, or magnesium compromise bone and muscle health.
Addressing these modifiable factors is essential for long-term pain relief and spinal health, complementing clinical treatments and physical therapy.
When to Seek Advanced Imaging
While X-rays are an important first step, there are situations where advanced imaging becomes necessary to detect hidden causes of chronic lower back pain:
- Pain that persists beyond 6-12 weeks despite conservative care
- Numbness, tingling, or weakness in the legs
- Pain that radiates below the knee
- Bowel or bladder changes, which may indicate nerve compression
- History of trauma, infection, or cancer
MRI or CT scans can reveal soft tissue injuries, early disc degeneration, nerve compression, or subtle inflammatory changes that X-rays cannot detect. Consulting a specialist for advanced imaging ensures hidden problems are not overlooked.
Comprehensive Approach to Chronic Lower Back Pain
Because many causes of chronic lower back pain are invisible on X-rays, effective management requires a multifaceted, patient-centered approach. Treating pain solely based on imaging can miss critical underlying factors. A comprehensive strategy typically includes:
- Medical evaluation: A thorough history and physical examination remain the cornerstone of diagnosis. Advanced imaging such as MRI or CT may be indicated if conservative treatment fails or if red-flag symptoms are present.
- Physical therapy: Targeted programs that include strengthening, stretching, and movement retraining help restore proper biomechanics, improve spinal stability, and reduce pain recurrence.
- Pain management: Nonsteroidal anti-inflammatory drugs (NSAIDs), topical analgesics, or nerve-targeted interventions can help control symptoms while addressing underlying causes.
- Lifestyle optimization: Exercise, posture correction, proper sleep habits, and nutrition support overall spinal health and accelerate recovery.
- Psychological support: Mind-body interventions, including cognitive-behavioral therapy (CBT), mindfulness meditation, and biofeedback, can reduce central sensitization and help patients cope with chronic pain.
- Alternative therapies: Acupuncture, massage therapy, and chiropractic care may provide additional relief, depending on individual response and the supporting evidence.
Research consistently shows that active, multidisciplinary management yields superior outcomes compared to isolated treatments, particularly when X-rays fail to reveal structural abnormalities. The focus shifts from simply treating symptoms to addressing the multiple, often hidden factors that contribute to chronic pain.
Prevention and Long-Term Strategies
Preventing chronic lower back pain or reducing its recurrence, requires consistent, proactive care. Patients who adopt long-term strategies experience better functional outcomes and less reliance on medical interventions. Key preventive measures include:
- Strengthen core and spinal stabilizers: Exercises like planks, bridges, and targeted back-strengthening routines improve spinal support and reduce stress on vulnerable structures.
- Maintain flexibility: Yoga, Pilates, or guided stretching programs help maintain range of motion and reduce muscle stiffness.
- Ergonomics: Proper workstation setup, lifting techniques, and posture awareness minimize cumulative strain on the spine.
- Regular physical activity: Low-impact exercises such as walking, swimming, cycling, or resistance training support overall spinal health and enhance circulation.
- Weight management: Maintaining a healthy weight reduces mechanical load on the lower back.
- Address underlying conditions early: Early detection and treatment of arthritis, disc degeneration, or inflammatory disorders can prevent chronic complications.
By prioritizing functional health, movement, and lifestyle adjustments, patients can often prevent severe chronic pain, even when imaging results are inconclusive. Prevention is not just about avoiding pain, it is about empowering patients to take control of their spinal health.
Key Takeaways
Chronic lower back pain is often misunderstood and underdiagnosed, especially when X-rays appear normal. Understanding the complexity of pain is essential for effective management. Key points to remember include:
- X-rays reveal bones, not soft tissue: Muscles, ligaments, discs, fascia, and nerves may harbor problems that X-rays cannot detect.
- Invisible causes matter: Chronic pain may stem from disc degeneration, muscle strain, ligament injury, nerve irritation, or myofascial dysfunction.
- Psychological, biomechanical, and lifestyle factors significantly influence pain perception, persistence, and recovery.
- Advanced imaging and multidisciplinary care are essential when pain persists despite normal X-rays.
- Prevention is critical: Exercise, proper posture, ergonomics, and healthy lifestyle choices can reduce the risk of recurrence and enhance overall spinal health.
Perhaps the most empowering lesson is that pain does not always equal visible damage. Recognizing this shifts the focus from a purely structural perspective to a holistic, evidence-based approach, one that addresses the root causes of discomfort, supports long-term wellness, and improves quality of life.
Final Thoughts
Chronic lower back pain can feel mysterious and isolating, especially when doctors tell you, “Your X-rays are fine.” However, the absence of visible damage does not mean the pain is not real or untreatable. By examining muscle health, disc integrity, nerve function, posture, and lifestyle factors, patients can uncover the underlying causes of their discomfort and develop strategies to regain function.
Modern science recognizes that chronic lower back pain is rarely the result of a single factor. Instead, it arises from a complex interplay of structures, nerves, and behaviors. Effective management requires a comprehensive approach, combining medical evaluation, physical therapy, lifestyle optimization, and psychological support with the right assessment, active interventions, and preventive strategies, it is entirely possible to restore mobility, reduce pain, and improve quality of life. Lower back pain may be invisible on X-rays, but with knowledge, targeted care, and proactive habits, it doesn’t have to remain invisible in your life.
Other Blog Post You Might Like:
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


