Why Wounds Heal Slowly in Diabetes: 10 Proven Biological Failures Explained
⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
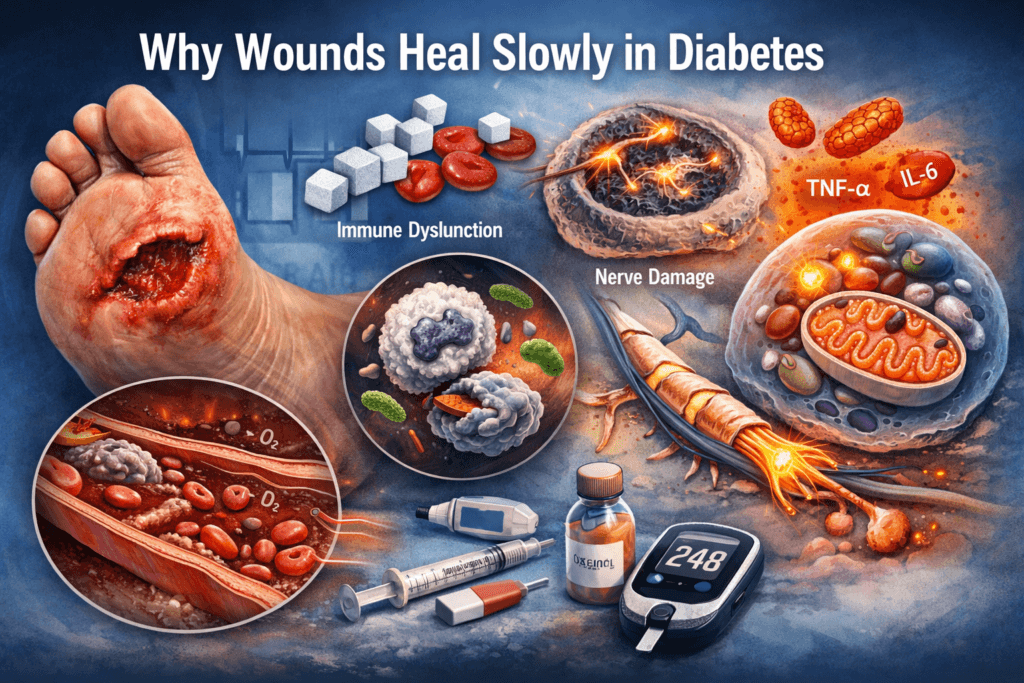
Wound healing is not a single event, it is a highly coordinated biological process that depends on intact blood vessels, responsive immune cells, functional nerves, sufficient oxygen delivery, and tightly regulated glucose metabolism.
Diabetes disrupts every one of these systems simultaneously. As a result, wounds in diabetes do not merely heal more slowly, they heal inefficiently, unpredictably, and with a significantly higher risk of infection, breakdown, and progression to chronic injury.
This is not coincidence or bad luck, it is the direct outcome of metabolic and vascular dysfunction acting at the cellular, immune, vascular, and neurological levels.
This section explains exactly how and why that disruption occurs, step by step.
The Normal Wound-Healing Process (What Should Happen)
To understand why wounds fail to heal in diabetes, you must first understand how healing works when metabolism and circulation are intact.
Wound healing is not automatic, it is a precisely timed biological cascade that requires coordination between blood vessels, immune cells, connective tissue, and skin cells.
When any part of this sequence is disrupted, healing slows. When multiple parts are disrupted as in diabetes, healing can fail entirely. Under normal conditions, wound healing progresses through four tightly coordinated phases.
1. Hemostasis (Minutes to Hours)
Immediately after injury:
- Blood vessels constrict to limit blood loss
- Platelets aggregate at the injury site
- A fibrin clot forms to seal the wound
This clot is not just a plug,
it is a temporary biological scaffold that releases growth factors and signals the immune system to begin repair. If hemostasis is unstable, the entire healing process becomes delayed from the start.
2. Inflammation (Hours to Days)
Once bleeding is controlled, the immune phase begins.
- Neutrophils migrate into the wound
- Bacteria and debris are destroyed
- Macrophages clear dead tissue and coordinate repair signals
Inflammation is essential but temporary, its job is cleanup not reconstruction. In healthy healing, inflammation peaks early and then resolves, allowing the wound to move forward.
3. Proliferation (Days to Weeks)
This is the rebuilding phase.
- New blood vessels form (angiogenesis)
- Fibroblasts produce collagen and extracellular matrix
- Keratinocytes migrate to close the wound surface
The wound begins to shrink, strengthen, and re-epithelialize. This phase is energy-intensive and highly dependent on:
- Oxygen delivery
- Growth factor signaling
- Adequate blood flow
4. Remodeling (Weeks to Months)
In the final phase:
- Collagen fibers reorganize and strengthen
- Excess blood vessels regress
- Scar tissue matures and stabilizes
The goal is not just closure but durable tissue integrity.
The Critical Point
Each phase depends on:
- Adequate circulation
- Oxygen availability
- Functional immune response
- Effective cellular signaling
- Sufficient metabolic energy
Diabetes interferes with every single one of these requirements.
The Core Problem: Chronic Hyperglycemia Damages the Healing Machinery
High blood sugar is often misunderstood as a passive excess. It is not.
Chronic hyperglycemia represents a toxic metabolic state that alters cellular behavior, damages blood vessels, and distorts immune function.
Over time, it causes:
- Progressive vascular injury
- Immune system dysfunction
- Nerve damage
- Persistent inflammatory signaling
- Mitochondrial and cellular energy failure
Healing does not stop but it becomes biologically inefficient, disorganized, and fragile. The wound environment shifts from regenerative to hostile.
1. Blood Vessel Damage: The Foundation Is Cracked
Why Blood Flow Is Non-Negotiable
Healing tissue is metabolically demanding.
It requires a constant supply of:
- Oxygen
- Glucose and amino acids
- Immune cells
- Growth factors and signaling molecules
All of these are delivered through healthy, responsive blood vessels, without adequate perfusion, healing cannot progress beyond early stages.
What Diabetes Does to Blood Vessels
Chronic hyperglycemia leads to progressive microvascular damage through multiple mechanisms:
- Endothelial dysfunction
The inner lining of blood vessels loses its ability to regulate flow and respond to signals. - Basement membrane thickening
Nutrient and oxygen exchange across capillaries becomes inefficient. - Capillary narrowing and rarefaction
Fewer functional vessels reach the wound. - Reduced nitric oxide production
Blood vessels lose the ability to dilate appropriately. - Impaired vasodilation
Flow cannot increase when tissue demand rises.
The Result, blood reaches the wound:
- More slowly
- In lower volume
- With reduced oxygen content
Clinically, diabetic wounds often appear:
- Pale
- Cool to touch
- Dry
- Poorly perfused
Without sufficient blood flow, tissue regeneration cannot be sustained.
Healing stalls at the foundation.
2. Oxygen Starvation: Healing Cannot Happen in Hypoxia
Oxygen is not optional in wound repair.
It is required for:
- Collagen synthesis
- Fibroblast proliferation
- Angiogenesis
- Bacterial killing by immune cells
How Diabetes Creates Local Hypoxia
Even when blood glucose appears moderately controlled, diabetes impairs oxygen delivery through:
- Microvascular disease limiting perfusion
- Reduced red blood cell deformability
- Impaired oxygen diffusion across thickened capillary walls
The wound may receive blood but not usable oxygen.
Clinical Consequences
Without adequate oxygen:
- Collagen production weakens
- New vessels fail to mature
- Immune cells lose bactericidal efficiency
This is why diabetic wounds often:
- Stall after initial closure
- Reopen repeatedly
- Break down under minimal stress
The problem is not effort, it is oxygen deprivation.
3. Immune Dysfunction: Defense Without Precision
Normal Immune Response in Healing
In metabolically healthy individuals:
- Neutrophils arrive quickly and accurately
- Macrophages clear debris and orchestrate repair
- Inflammation resolves once its job is done
This controlled response clears infection without damaging healthy tissue.
How Diabetes Disrupts Immune Cells
Chronic hyperglycemia alters immune cell behavior at multiple levels:
- Neutrophil dysfunction
Cells become slower and less effective. - Reduced chemotaxis
Immune cells fail to reach the wound in adequate numbers. - Impaired phagocytosis
Bacteria and debris are cleared inefficiently. - Delayed macrophage activation
Repair signals are weakened and poorly timed.
The Result:
- Bacteria persist longer
- Inflammation fails to resolve
- Tissue damage accumulates
This explains why diabetic wounds are:
- Easily infected
- Slow to clear infection
- Prone to chronic, non-resolving inflammation
The immune system is present but poorly coordinated.
4. Chronic Inflammation: When the Healing Process Gets Stuck
Inflammation is a tool, not a destination, in normal wound healing, inflammation:
- Activates rapidly
- Performs cleanup
- Resolves once repair begins
In diabetes, that resolution fails.
Why Diabetes Keeps Inflammation Turned On
Chronic hyperglycemia creates a persistent pro-inflammatory environment through several overlapping mechanisms:
- Excess cytokine release
Elevated levels of TNF-α, IL-6, and other inflammatory mediators continuously signal tissue damage even when repair should be underway. - Oxidative stress
High glucose increases reactive oxygen species, which damage cell membranes, proteins, and DNA. - Advanced glycation end-products (AGEs)
Glucose binds irreversibly to proteins and lipids, altering their structure and function.
How AGEs Actively Block Healing
AGEs are not passive byproducts. They actively interfere with repair by:
- Damaging structural and signaling proteins
- Stiffening tissue and extracellular matrix
- Disrupting cell-to-cell communication
Instead of transitioning from inflammation to proliferation, the wound becomes locked in an inflammatory loop. The Result, chronic wounds are not weak wounds they are biologically stalled wounds, trapped in a phase they are meant to leave.
5. Impaired Collagen Production: The Structural Scaffold Is Weak
Collagen is the primary structural protein responsible for:
- Wound closure
- Tensile strength
- Long-term tissue stability
Without healthy collagen, wounds may close superficially but lack durability.
How Diabetes Disrupts Collagen Formation
Diabetes interferes with collagen integrity in three critical ways:
- Reduced fibroblast activity
Fibroblasts become less responsive to growth signals and produce less collagen. - Abnormal collagen cross-linking
Collagen fibers fail to organize properly, weakening tissue strength. - AGE-modified collagen
Glycation makes collagen brittle, disorganized, and resistant to normal remodeling.
Clinical Consequences
As a result:
- Wounds close more slowly
- Scar tissue is fragile
- Re-injury occurs with minimal stress
This explains why diabetic wounds may appear healed, only to reopen weeks or months later.
6. Impaired Angiogenesis: New Blood Vessels Fail to Form
Healing cannot progress without new blood vessel formation.
Angiogenesis supplies:
- Oxygen
- Nutrients
- Immune cells
- Growth factors
Without it, repair stalls.
How Diabetes Blocks Angiogenesis
Chronic hyperglycemia reduces:
- VEGF (vascular endothelial growth factor):
The primary signal for new vessel formation. - Endothelial progenitor cell function:
Fewer repair-capable cells are available to build new vessels. - Nitric oxide signaling:
Blood vessels lose responsiveness and adaptability.
The Result, without adequate angiogenesis:
- Tissue remains chronically under-oxygenated
- Nutrient delivery is insufficient
- Healing plateaus despite treatment
This is particularly devastating in:
- Diabetic foot ulcers
- Surgical wounds
- Pressure injuries
7. Neuropathy: Wounds Begin Unnoticed and Progress Untreated
One of the most dangerous contributors to chronic wounds in diabetes is loss of sensation.
What Diabetic Neuropathy Causes
- Reduced or absent pain perception
- Pressure points go unnoticed
- Minor injuries receive no early care
Pain normally serves as a protective signal, in diabetes, that signal is muted or absent.
How Small Injuries Become Major Wounds
A minor blister:
- Is not felt
- Is not offloaded
- Is not treated
It progresses into:
- An ulcer
- Then an infection
- Then necrosis
By the time intervention begins, the wound environment is already severely compromised. This is why diabetic foot ulcers are not sudden events.
They are missed early injuries that evolve silently.
8. High Glucose Actively Feeds Infection
Bacteria thrive in glucose-rich environments, hyperglycemia does not merely weaken defenses, it actively supports microbial growth.
How High Glucose Promotes Infection
- Increases bacterial replication
- Weakens local immune responses
- Reduces penetration and effectiveness of antibiotics
Infection Worsens the Healing Environment
Once infection takes hold, it:
- Amplifies inflammation
- Destroys viable tissue
- Further impairs circulation
This creates a self-perpetuating cycle:
High glucose causes infection then inflammation leading to tissue damage and delayed healing.
9. Reduced Growth Factor Signaling: Repair Instructions Are Weakened
Growth factors act as the instruction manual for healing.
They tell cells when to:
- Migrate
- Divide
- Differentiate
- Repair
How Diabetes Disrupts Growth Factor Action
Diabetes reduces both the availability and effectiveness of key growth factors, including:
- PDGF (platelet-derived growth factor)
- TGF-β (transforming growth factor-beta)
- EGF (epidermal growth factor)
Cells receive weaker, delayed, or distorted repair signals.
The Result, healing becomes:
- Disorganized
- Incomplete
- Inefficient
The wound lacks coordinated progression from one phase to the next.
10. Cellular Energy Failure: Repair Without Fuel
Healing is energy-intensive.
Cells require ATP to:
- Divide
- Migrate
- Produce proteins
- Remodel tissue
How Diabetes Starves Healing Cells
Despite high blood glucose, diabetes causes:
- Mitochondrial dysfunction
- Insulin resistance within repair cells
- Impaired glucose uptake where it is most needed
The Central Paradox
Blood sugar is high.
Healing cells are energy-starved. Repair slows not because resources are absent but because they are unusable.
Why Diabetic Wounds Become Chronic
A wound becomes chronic when:
- Blood flow is inadequate
- Inflammation does not resolve
- Infection persists
- Cellular repair mechanisms fail
Diabetes meets every one of these conditions simultaneously.
The Outcome
That is why diabetic wounds:
- Persist for months or years
- Require advanced and multidisciplinary care
- Sometimes never fully heal
This is not poor wound care.
It is predictable pathophysiology.
Why Amputation Risk Exists
Amputation is often framed as an unavoidable complication of diabetes.
That framing is incorrect.
Diabetes itself does not remove limbs, what leads to amputation is the accumulation of late-stage failures that follow prolonged, uncorrected biological dysfunction.
Amputation occurs when one or more of the following processes become irreversible:
- Non-healing wounds that fail to close despite care
- Progressive infection that penetrates deeper tissues and bone
- Ischemia from critically impaired blood supply
- Tissue necrosis resulting from oxygen and nutrient deprivation
Once viable tissue cannot be preserved, removal becomes the only option to prevent systemic infection and death. Amputation, therefore, is not an early failure of care.
It is a late-stage consequence of prolonged vascular, immune, and metabolic breakdown.
What Actually Improves Healing in Diabetes (Evidence-Based)
There is no shortcut, supplement, or topical treatment that overrides impaired biology. Only interventions that correct the underlying metabolic and vascular environment improve healing outcomes. The evidence is clear.
1. Tight, Stable Glucose Control
Healing improves with stable glucose levels, not simply a lower average.
- Reduced glucose variability limits inflammatory spikes
- Lower oxidative stress protects blood vessels
- Immune function improves as hyperglycemic toxicity declines
HbA1c alone is insufficient if daily swings remain severe.
2. Early Detection
Timing determines outcome.
- Daily foot inspection identifies injuries before progression
- Immediate attention to any break in the skin prevents escalation
Most diabetic amputations begin with a wound that went unnoticed or untreated early.
3. Vascular Assessment
Healing cannot occur without blood flow.
- Peripheral circulation must be evaluated early
- Ischemia must be identified before tissue death occurs
Treating a wound without assessing perfusion is biologically ineffective.
4. Pressure Offloading
Mechanical stress impairs healing even in healthy tissue.
In diabetes:
- Continuous pressure worsens ischemia
- Repetitive trauma reopens fragile wounds.
Offloading is essential, particularly for plantar foot ulcers.
5. Aggressive Infection Control
Infection accelerates tissue destruction.
- Early identification limits spread
- Prompt, targeted treatment prevents deeper invasion
- Delayed response dramatically increases amputation risk
In diabetes, waiting is not neutral, it is damaging.
6. Nutritional Support
Healing requires raw materials.
- Adequate protein supports collagen synthesis
- Micronutrients enable immune and enzymatic function
- Caloric sufficiency prevents catabolism
Malnutrition silently undermines wound repair, even with good glucose control.
7. Multidisciplinary Care
Diabetic wound healing is not a single-specialty problem.
Optimal outcomes require coordination between:
- Endocrinology (metabolic control)
- Podiatry (mechanical and structural care)
- Vascular specialists (perfusion)
- Wound care teams (local management)
Fragmented care leads to fragmented healing.
The Bottom Line, healing in diabetes improves only when:
- Metabolism is stabilized
- Circulation is preserved
- Infection is controlled
- Mechanical stress is removed
- Repair is supported systemically
Anything less manages symptoms, not outcomes.
The Final Truth
Wounds heal slowly in diabetes because the entire biological repair system is impaired. This is not chance, this is not bad care, this is predictable pathophysiology.
Diabetes progressively damages:
- Blood vessels that deliver oxygen and nutrients
- Immune responses that clear infection and coordinate repair
- Nerves that signal injury early
- Cellular energy systems required for regeneration
- Inflammatory control mechanisms that allow healing to advance
As a result, tissue repair is forced to occur in an environment that is structurally, metabolically, and immunologically hostile to healing.
Delayed healing is not a failure of effort, it is the expected outcome of untreated or late-treated metabolic dysfunction. Early metabolic control preserves healing capacity, late intervention manages accumulated damage.
💡 Expert Guidance at Your Fingertips
Speak with a licensed doctor from MuseCare Consult and get actionable advice for your health questions, labs, or medications, all online and secure.
💬 Start Your ConsultationMust Read:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- Can Diabetes Be Reversed? 7 Science-Backed Facts You Must Know
- 7 Alarming Ways Heart Disease and Diabetes Are Secretly Linked
- 10 Powerful Steps Showing How Diabetic Kidney Disease Develops and Progresses
- 10 Critical Reasons Why Diabetes Damages Blood Vessels Before Symptoms Appear
- Diabetic Neuropathy Explained: 12 Brutal Reasons High Sugar Destroys Nerves
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


