10 Powerful Steps Showing How Diabetic Kidney Disease Develops and Progresses
⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
Diabetic kidney disease does not arrive suddenly, it does not announce itself with pain, warning signs, or dramatic symptoms and it is not the result of bad luck, aging, or an unfortunate turn of events. It is the predictable outcome of a process that has been unfolding quietly for years.
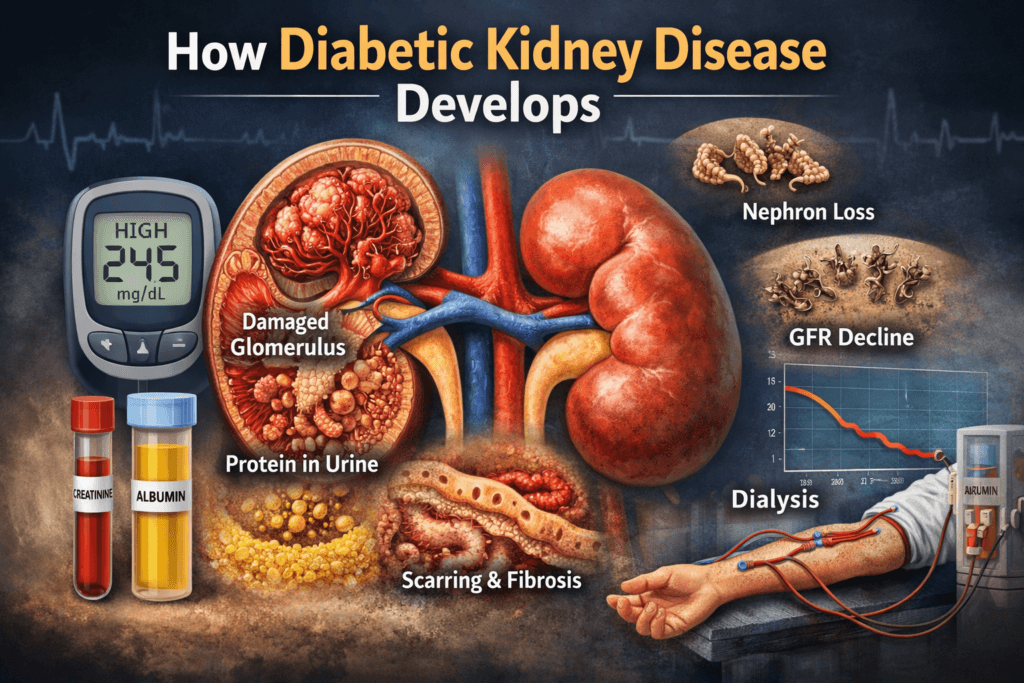
By the time creatinine rises, by the time protein appears consistently in urine, by the time dialysis is even mentioned, the disease is no longer beginning, it is well established. The critical damage has already occurred, unseen and unrecognized, at a microscopic level where standard symptoms do not exist.
The earliest injury happens inside the kidney’s smallest structures, the glomeruli and filtration cells responsible for cleaning the blood. These structures are exquisitely sensitive to metabolic stress. Long before diabetes is formally diagnosed, long before glucose crosses diagnostic thresholds, these cells are already being exposed to abnormal pressure, inflammation, and chemical injury.
This is why diabetic kidney disease is so often described as sudden or unexpected. The damage is not sudden, the detection is late.
To understand how diabetes leads to kidney disease, one dangerous misconception must be abandoned, the idea that diabetes is simply a condition of high blood sugar. Elevated glucose is not the disease itself, it is a visible signal of deeper metabolic and vascular failure. The real injury occurs through disrupted blood flow regulation, chronic inflammation, oxidative stress, and sustained pressure inside fragile kidney filters.
Seen through this lens, diabetic kidney disease stops being mysterious, it becomes logical, stepwise. mechanistic and, importantly, largely predictable.
What follows is not a list of complications, but a biological sequence, how years of metabolic dysfunction translate into irreversible structural damage, one stage at a time.
Step 1: Chronic Hyperglycemia Injures the Kidney’s Microvasculature
The kidneys filter blood through microscopic structures called glomeruli,
each kidney contains roughly one million of these filters, and each glomerulus is a dense knot of fragile capillaries designed for precision, not stress.
These vessels are among the most glucose-sensitive blood vessels in the body, when blood sugar remains elevated even modestly, even intermittently, the injury begins at the molecular level.
Several damaging processes are triggered simultaneously:
- Glucose binds irreversibly to proteins and lipids, forming advanced glycation end products (AGEs)
- AGEs accumulate in vessel walls, making them thicker, stiffer, and less responsive
- Nitric oxide production falls, impairing vasodilation and normal blood flow regulation
- Oxidative stress increases, damaging cellular structures and DNATogether, these changes produce endothelial dysfunction, the inner lining of the kidney’s blood vessels loses its ability to regulate pressure, flow, and filtration properly.
This is not a late complication. it is an early metabolic injury.
In many people, this damage begins years before diabetes is diagnosed, often during insulin resistance or prediabetes, when blood sugar levels are still considered borderline or acceptable. Lab results may look reassuring, the kidneys are not.
Step 2: Increased Pressure Inside the Glomerulus (Hyperfiltration)
In the early stages of diabetes, the kidneys respond to excess glucose by working harder. They begin filtering more blood than normal, a phenomenon known as glomerular hyperfiltration. This response is often misunderstood as a sign of strong kidney function, it is not, it is a compensatory stress response.
Here is the mechanism:
- High glucose levels cause dilation of the afferent arteriole, the vessel bringing blood into the glomerulus
- The efferent arteriole does not dilate to the same degree
- Pressure inside the glomerular capillary bed rises
- Filtration increases beyond physiologic safety limits
The result is sustained high-pressure flow through structures that were never designed to withstand it. A useful analogy is forcing a fragile paper filter to process double its intended volume continuously. It works for a while but at the cost of structural integrity.
During this phase:
- Estimated GFR may appear high or excellent
- Serum creatinine often remains normal
- Patients are told their kidneys are functioning well
In reality, this phase accelerates microscopic injury and sets the stage for permanent damage.
Hyperfiltration is one of the strongest early predictors of future kidney failure, not a sign of health.
Step 3: Damage to the Glomerular Basement Membrane
The glomerulus filters blood using a highly specialized three-layer barrier:
- Endothelial cells lining the capillaries
- The glomerular basement membrane (GBM)
- Podocytes, which form the final filtration layer
Chronic hyperglycemia disrupts this architecture.
The basement membrane becomes:
- Abnormally thickened
- Less flexible
- Chemically altered by glycation and oxidative injury
As a result:
- Filtration loses its selectivity
- Structural resilience declines
- The barrier begins to leak
Albumin, a vital blood protein that should remain in circulation, starts passing into the urine. Initially, this leakage is small and inconsistent, it may only appear during illness, exercise, or periods of poor glucose control. This stage is labeled microalbuminuria.
The label is misleading, microalbuminuria does not mean minimal disease.
It means structural kidney damage is already present. Once proteins cross the filtration barrier, the integrity of the system has already been compromised.
Step 4: Podocyte Injury and Loss (The Turning Point)
Podocytes are highly specialized cells that wrap around glomerular capillaries and maintain the final barrier preventing protein loss. They are critical and fragile.
Unlike many other cell types, podocytes have very limited capacity to regenerate.
Chronic high glucose injures podocytes through multiple converging mechanisms:
- Persistent oxidative stress damages cellular structures
- Inflammatory signaling disrupts normal function
- Mechanical strain from hyperfiltration stretches and destabilizes the cells
- AGEs accumulate, impairing cellular adhesion and survival
Over time, podocytes detach from the basement membrane or undergo cell death.
Once this happens:
- Filtration becomes permanently compromised
- Protein leakage accelerates
- Structural collapse of the glomerulus begins
This marks a critical transition. At this point, treatment can slow progression, reduce pressure, and limit further loss but it cannot reliably replace lost podocytes or fully restore normal filtration.
This is the stage where diabetic kidney disease shifts from functional disturbance to irreversible structural injury.
And importantly, it often occurs while kidney function tests still appear near normal.
Step 5: Persistent Proteinuria Triggers Inflammation and Scarring
Protein in the urine is not just a marker, it is toxic to kidney tissue. When protein leaks into renal tubules:
- Tubular cells become inflamed
- Immune signaling is activated
- Fibrotic pathways turn on
This leads to:
- Tubulointerstitial inflammation
- Progressive scarring (fibrosis)
- Loss of functional kidney tissue
At this stage:
- Albuminuria becomes persistent
- Blood pressure often rises
- Kidney damage accelerates even if glucose improves
This is why early control matters far more than late correction.
Step 6: Activation of the Renin-Angiotensin-Aldosterone System (RAAS)
Diabetic kidney damage activates the RAAS system, which regulates blood pressure and fluid balance.
Chronic activation causes:
- Vasoconstriction of kidney vessels
- Increased glomerular pressure
- Sodium and water retention
- Worsening hypertension
High blood pressure then:
- Further damages glomeruli
- Accelerates protein leakage
- Creates a vicious feedback loop
Diabetes causes kidney damage which leads to hypertension then faster kidney damage. This is why ACE inhibitors and ARBs are protective, not because they lower sugar, but because they reduce intraglomerular pressure.
Step 7: Progressive Loss of Nephrons
Each kidney contains about one million nephrons at birth, they do not regenerate.
As diabetic damage progresses:
- Individual nephrons scar and fail
- Remaining nephrons compensate by hyperfiltering
- Compensation accelerates their own damage
This creates a self-amplifying cycle:
- Fewer working nephrons
- Higher pressure per nephron
- Faster decline in kidney function
This is why kidney decline often accelerates in later stages.
Step 8: Decline in Glomerular Filtration Rate (GFR)
Eventually, compensation fails.
GFR begins to fall:
- Waste products accumulate
- Fluid regulation worsens
- Electrolyte balance becomes unstable
At this point:
- Creatinine rises
- eGFR drops below normal
- Symptoms may begin to appear
But understand this:
By the time GFR declines, decades of injury may have already occurred. Kidney disease is diagnosed late because the kidneys are silent organs.
Step 9: Structural Remodeling and Fibrosis
Chronic diabetes transforms kidney architecture:
- Normal tissue is replaced with scar tissue
- Capillary networks collapse
- Oxygen delivery decreases
- Inflammation becomes chronic
Fibrosis is the final common pathway of kidney failure.
Once fibrosis dominates:
- Damage becomes largely irreversible
- Treatment focuses on slowing, not reversing
Step 10: End-Stage Kidney Disease (ESKD)
When kidney function falls below survival thresholds:
- Dialysis becomes necessary
- Or kidney transplantation is required
This is not a sudden event.
It is the end of a long biological process that often began 10-20 years earlier.
Why Many People Are Surprised by Diabetic Kidney Disease
Diabetic kidney disease is often described as unexpected or sudden. In reality, what is sudden is not the damage, it is the recognition of damage.
The medical system is structured to detect kidney failure late, not early. As a result, years of progressive injury pass unnoticed. Several systemic failures contribute to this false sense of surprise:
- Overreliance on late markers such as serum creatinine and eGFR, which change only after substantial nephron loss
- Failure to recognize hyperfiltration as an early warning sign rather than a sign of healthy kidneys
- Neglect of insulin resistance and metabolic dysfunction before diabetes is formally diagnosed
- Underestimation of microalbuminuria, which is often mislabeled as mild or reversible
Diabetes care is largely reactive, intervention escalates only after measurable damage appears. The kidneys, which tolerate injury silently, absorb the cost of this delay.
Major Risk Factors That Accelerate Kidney Damage
Diabetic kidney disease does not progress at the same pace in everyone. However, the factors that accelerate decline are well established and consistent.
Risk increases substantially with:
- Poor glucose control marked by high variability, not just elevated averages
- Chronic hypertension, even when modest
- Smoking, which compounds vascular injury
- Obesity, which increases inflammatory and hemodynamic stress
- Genetic susceptibility affecting vascular and inflammatory responses
- Long duration of diabetes, regardless of current control
- Absence or delayed use of RAAS-blocking medications
- Late diagnosis of metabolic dysfunction
One misconception deserves emphasis, normal fasting glucose does not guarantee kidney safety. It may simply indicate that insulin compensation is still masking deeper dysfunction.
Kidney damage tracks exposure time and vascular stress, not a single laboratory value.
Can Diabetic Kidney Disease Be Reversed?
This question demands honesty, early in the disease process, when changes are primarily functional, improvement is possible. Hyperfiltration can normalize, albumin leakage can decrease, inflammatory signaling can quiet. Once structural damage dominates, reversal is no longer realistic.
What can be achieved:
- Tight and consistent glucose control
- Aggressive blood pressure management
- RAAS inhibition to reduce intraglomerular pressure
- Use of SGLT2 inhibitors to lower filtration stress and inflammation
- Sustained weight reduction
- Dietary sodium restriction
- Early and repeated screening
What cannot be achieved:
- Regeneration of lost nephrons
- Restoration of normal kidney architecture
- Complete reversal of fibrosis
This distinction matters, late, intensive treatment cannot substitute for early, decisive intervention. Timing determines outcome more than effort applied after damage is established.
The Core Truth Most People Miss
Diabetic kidney disease is often labeled a complication, as if it were optional or incidental, it is neither.
It is a predictable consequence of prolonged metabolic and vascular injury.
It does not begin when laboratory values cross abnormal thresholds, it begins when glucose regulation, blood flow control, and cellular resilience quietly fail.
Waiting for symptoms means waiting for advanced disease,
waiting for diagnosis means intervening after injury is entrenched.
Understanding this timeline is not pessimism, it is the difference between prevention and damage control and that distinction determines everything.
Final Truth
Diabetes does not damage the kidneys in a single dramatic moment, it does so incrementally, vessel by vessel, cell by cell, year after year. The process is silent because the kidneys are resilient, it is progressive because metabolic injury does not pause.
It is largely preventable early because structure has not yet been lost and it is largely irreversible late because scar tissue cannot be undone. Kidney failure is not the beginning of diabetic kidney disease, it is the endpoint, the visible conclusion of a biological timeline that was unfolding long before symptoms, long before abnormal labs, and often long before diagnosis.
By the time kidney failure becomes obvious, the decisive moments have already passed, what remains is management, not rescue. This is why early understanding is not academic, it is protective,
it allows intervention while filtration structures still exist, while pressure can still be reduced, while inflammation has not yet hardened into fibrosis.
Late awareness offers no such advantage, it can slow decline, reduce suffering, and extend time but it cannot restore what has been structurally lost.
There is no sugarcoating this reality because biology does not negotiate, diabetic kidney disease follows rules, not intentions. Ignore the early signals, and the kidneys absorb the damage quietly.
Recognize the process early, and progression can be altered, that is the difference between prevention and damage control, it is the only difference that truly matters.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Blog Post:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- 10 Critical Reasons Why Diabetes Damages Blood Vessels Before Symptoms Appear
- Diabetic Neuropathy Explained: 12 Brutal Reasons High Sugar Destroys Nerves
- 7 Critical Reasons Continuous Glucose Monitoring Can Transform Your Health
- Why Normal Blood Sugar Readings Can Still Hide Diabetes: 10 Shocking Truths You Must Know
- 10 Critical Insights Into Blurred Vision in Diabetes: Temporary Changes vs Dangerous Damage
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


