⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
Most people think of blood sugar as a single number, the one they see on a fasting test or a fingerstick reading. The truth is far more complex, blood sugar rises and falls constantly throughout the day, influenced by what you eat, how you move, how you sleep, and even how stressed you are.
For decades, we have relied on snapshots, fasting blood sugar, random checks, or three month averages to assess metabolic health. These methods are not useless, but they are limited, they miss the patterns that reveal early dysfunction and hidden risk.
Metabolic problems do not appear suddenly, they creep in, hour by hour, day by day. Continuous glucose monitoring captures these subtle changes in real time, exposing what traditional tests cannot.
The question is not whether continuous monitoring works. The real question is, who actually needs it and why it matters more than you think.
What Continuous Glucose Monitoring Really Is
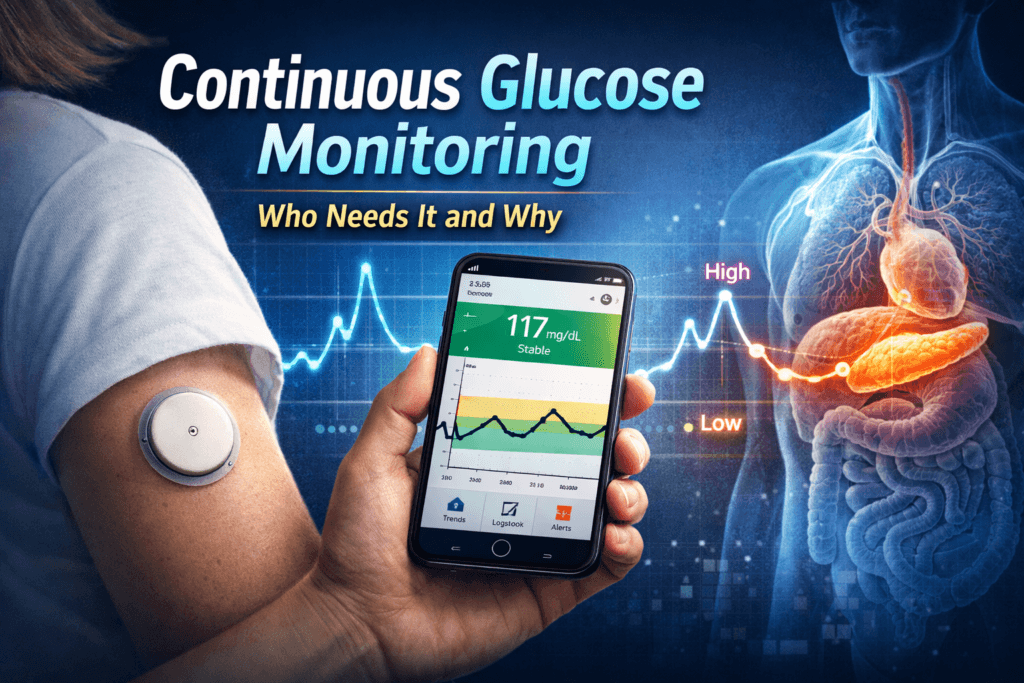
Continuous glucose monitoring is a method of measuring blood sugar levels throughout the day and night using a small sensor placed just under the skin. Unlike traditional methods that give a single reading at one point in time, this technology continuously tracks glucose levels in the fluid surrounding the cells, providing a comprehensive picture of how the body handles sugar.
Continuous monitoring does more than give a number. It provides:
- Regular readings every few minutes to reveal fluctuations that would otherwise go unnoticed
- Trends showing whether glucose is rising or falling, helping anticipate spikes or drops before they become dangerous
- Daily glucose curves that illustrate patterns across meals, activity, and sleep
- Information about time spent within healthy ranges, offering a clearer view of overall metabolic control
- Alerts for high or low glucose levels, allowing early intervention before complications arise
This approach transforms glucose monitoring from reactive to proactive. Instead of asking, “What is my glucose right now?” the question becomes, “How is my glucose behaving throughout the day?” This shift provides insights into the body’s responses to meals, exercise, stress, and sleep, information that static tests simply cannot capture.
The Key Differences Between Fingerstick Testing and Continuous Monitoring
Fingerstick Testing:
Traditional fingerstick tests measure blood sugar at a single moment, they are useful for confirming a reading or checking fasting levels but have significant limitations:
- They cannot reveal how glucose has changed over the previous hours
- They cannot predict whether glucose is rising or falling
- They cannot capture spikes or drops that occur between tests
In short, fingerstick tests provide points. They do not reveal the bigger picture of metabolic health.
Continuous Monitoring:
Continuous monitoring, on the other hand, captures patterns, not just points. It reveals:
- How meals affect glucose, showing which foods cause prolonged spikes and which have minimal impact
- How physical activity influences blood sugar, highlighting which exercises stabilize or destabilize glucose levels
- How sleep and stress affect glucose, identifying nighttime spikes or morning highs caused by hormonal fluctuations
- Hidden post-meal spikes, which may appear normal in fasting tests but indicate early dysfunction
- Medication or insulin effectiveness, enabling adjustments based on real-time feedback
Metabolic disease does not develop in isolated points, it develops in patterns. Continuous monitoring allows these patterns to be identified and addressed before long-term complications occur.
Who Benefits Most from Continuous Glucose Monitoring
Continuous glucose monitoring is often perceived as a luxury. In reality, it is a powerful tool for anyone whose glucose patterns cannot be accurately captured by traditional tests. The real question is not insurance coverage, it is who gains meaningful health benefits.
1. People with Type 1 Diabetes
For individuals who do not produce insulin naturally, continuous monitoring is essential. It allows for:
- Prevention of dangerous low blood sugar episodes
- Reduction in blood sugar variability
- Guidance for precise insulin dosing
- Protection against nighttime hypoglycemia
Without continuous monitoring, people with type 1 diabetes rely on intermittent checks that cannot fully prevent complications.
2. People with Insulin-Treated Type 2 Diabetes
Type 2 diabetes treated with insulin often involves unpredictable blood sugar responses due to fluctuating insulin resistance. Continuous monitoring helps by:
- Detecting both high and low blood sugar events
- Guiding safer insulin dosing and timing
- Preventing complications caused by undetected spikes or drops
For these individuals, relying solely on occasional fingerstick tests is insufficient for optimal management.
3. People with Recurrent Low Blood Sugar
Hypoglycemia is dangerous regardless of diabetes status. Continuous monitoring is particularly beneficial for:
- People with hypoglycemia unawareness
- Individuals experiencing low blood sugar after surgery or due to medications
- Anyone prone to sudden drops in blood sugar
By alerting users before dangerous lows occur, continuous monitoring allows early intervention and reduces the risk of severe events.
4. People with Normal Blood Sugar but Metabolic Risk
Even individuals with normal fasting blood sugar or average blood sugar readings may experience hidden spikes after meals or prolonged elevated glucose levels. Continuous monitoring identifies early dysfunction that standard tests cannot detect. Recognizing these patterns allows for preventive measures, such as dietary changes or lifestyle adjustments, to reduce long-term risk.
5. People with Prediabetes
Prediabetes is a warning, not a diagnosis. Continuous monitoring helps determine:
- Which meals or snacks cause unhealthy glucose rises
- How physical activity affects glucose regulation
- How daily habits influence overall glucose control
This data enables targeted interventions, making lifestyle changes more effective and measurable rather than relying on guesswork.
6. Athletes and Physically Active Individuals
Active individuals can benefit from continuous monitoring by understanding how training, recovery, and stress affect blood sugar. Benefits include:
- Preventing low blood sugar during or after exercise.
- Optimizing nutrition for performance and recovery.
- Recognizing how stress or fatigue impacts glucose.
It is important to interpret spikes and dips correctly, as not every fluctuation is harmful.
7. People with Metabolic Syndrome, Polycystic Ovary Syndrome, or Fatty Liver Disease
These conditions are often driven by hidden glucose dysregulation. Continuous monitoring can reveal:
- Early insulin resistance
- Sensitivity to certain carbohydrates
- Stress or hormone-related glucose spikes
- Nighttime or fasting glucose abnormalities
Even when standard tests appear normal, continuous monitoring exposes the subtle dysfunction that contributes to long-term health risks.
Why This Matters
Continuous monitoring is more than a convenience, it is a tool for early detection, targeted intervention, and prevention of long-term complications. By revealing hidden patterns, it allows people to understand how their body responds in real time and make informed decisions about diet, activity, and treatment.
Patterns, not snapshots, define metabolic health, continuous monitoring ensures that these patterns are visible, actionable, and ultimately, controllable.
What Continuous Monitoring Reveals That Standard Tests Cannot
While standard blood sugar tests provide valuable information, they only offer isolated snapshots. Continuous monitoring uncovers patterns and behaviors that are otherwise invisible, helping people understand their metabolic health at a deeper level.
Time in Healthy Range
Average blood sugar values can be misleading. Two people may have the same average reading, yet one may maintain stable glucose levels while the other experiences extreme highs and lows. Continuous monitoring tracks how long glucose stays within healthy ranges, offering a much clearer picture of metabolic stability. This metric allows people and clinicians to identify patterns that contribute to long-term complications and to focus on interventions that keep glucose within safe limits consistently.
Blood Sugar Variability
Frequent fluctuations in blood sugar are more than just numbers, they are linked to oxidative stress, inflammation, and increased risk of cardiovascular disease, standard tests cannot quantify this variability. Continuous monitoring measures how much and how often glucose swings throughout the day, highlighting hidden stress on the body and helping guide interventions to stabilize blood sugar. Reducing variability is often just as important as lowering average blood sugar.
Post-Meal Glucose Response
The body’s response after meals often reveals early signs of metabolic dysfunction. Continuous monitoring shows:
- How high glucose spikes rise after eating
- How long elevated levels persist
- How quickly glucose returns to baseline
These post-meal patterns provide insight into insulin sensitivity, carbohydrate tolerance, and overall metabolic health. Standard fasting tests or three month averages cannot detect these early warning signs, meaning problems may remain hidden until they worsen.
Who Might Not Need Continuous Monitoring
Continuous monitoring is a powerful tool, but it is not necessary for everyone. People who may not benefit include:
- Those with stable, well-controlled type 2 diabetes managed effectively with diet and lifestyle alone
- Individuals with no metabolic risk factors and consistently healthy blood sugar responses
- People who may become anxious or obsessive over glucose data
The key point is that data is only useful when it is interpreted correctly and acted upon appropriately, without context and understanding, continuous monitoring can create confusion rather than clarity.
Common Misunderstandings About Continuous Monitoring
Even though continuous monitoring is a valuable tool, several misconceptions persist:
- It does not replace standard blood tests. It complements them by providing dynamic insights, not static averages.
- It does not measure blood glucose directly. Instead, it measures glucose in the fluid surrounding the cells, which closely reflects blood sugar trends.
- Not all glucose spikes are harmful. The body naturally experiences fluctuations, and context such as meal composition and activity is essential for interpretation.
- It does not guarantee better control. Continuous monitoring provides information, but improvements in blood sugar depend on behavior, lifestyle adjustments, and correct interpretation.
Understanding these distinctions helps users maximize the benefits of continuous monitoring without misusing or misinterpreting the data.
The Psychological Impact
Continuous monitoring can be empowering. It allows people to see patterns, make informed decisions, and prevent complications. It can also:
- Increase awareness of how food, exercise, and stress affect glucose
- Motivate positive lifestyle changes
- Provide reassurance when glucose remains stable
However, continuous monitoring can also create anxiety or lead to unnecessary dietary restrictions if the data is misinterpreted. The true value lies in understanding the patterns, not fixating on individual numbers. When used thoughtfully, continuous monitoring becomes a tool for clarity and prevention rather than fear.
Conclusion: See the Patterns Before They Become Problems
Blood sugar is not a single number, it is a constantly shifting pattern. Traditional tests only capture snapshots, leaving critical fluctuations and early signs of dysfunction invisible. Continuous monitoring exposes these patterns in real time, giving people the information they need to act before complications arise.
It is not just for those with type 1 diabetes or insulin-treated type 2 diabetes. Anyone with recurrent low blood sugar, prediabetes, or early metabolic dysfunction can benefit from understanding how their body actually responds to food, activity, and daily stressors.
Waiting for a test to cross a diagnostic threshold is already too late, continuous monitoring provides the chance for early intervention, safer management, and prevention of long-term damage. Ignoring these dynamic patterns allows metabolic problems to progress quietly.
Continuous monitoring is not a luxury, it is a window into how the body truly works, empowering people to make informed choices, protect their health, and prevent irreversible harm.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowOther Blog Post You Might Like:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- How Blood Sugar Is Regulated in the Body: 10 Key Mechanisms Explained
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- Why Normal Blood Sugar Readings Can Still Hide Diabetes: 10 Shocking Truths You Must Know
- 10 Critical Insights Into Blurred Vision in Diabetes: Temporary Changes vs Dangerous Damage
- Fasting Blood Sugar vs HbA1c vs OGTT: 7 Critical Differences Every Patient Must Know
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


