⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
You’re reading a book, scrolling on your phone, or driving home and suddenly, the world around you seems out of focus, letters blur together, street signs fuzz, faces lose their sharp edges. For a moment, you think it’s just fatigue or a long day but then you remember you have diabetes.
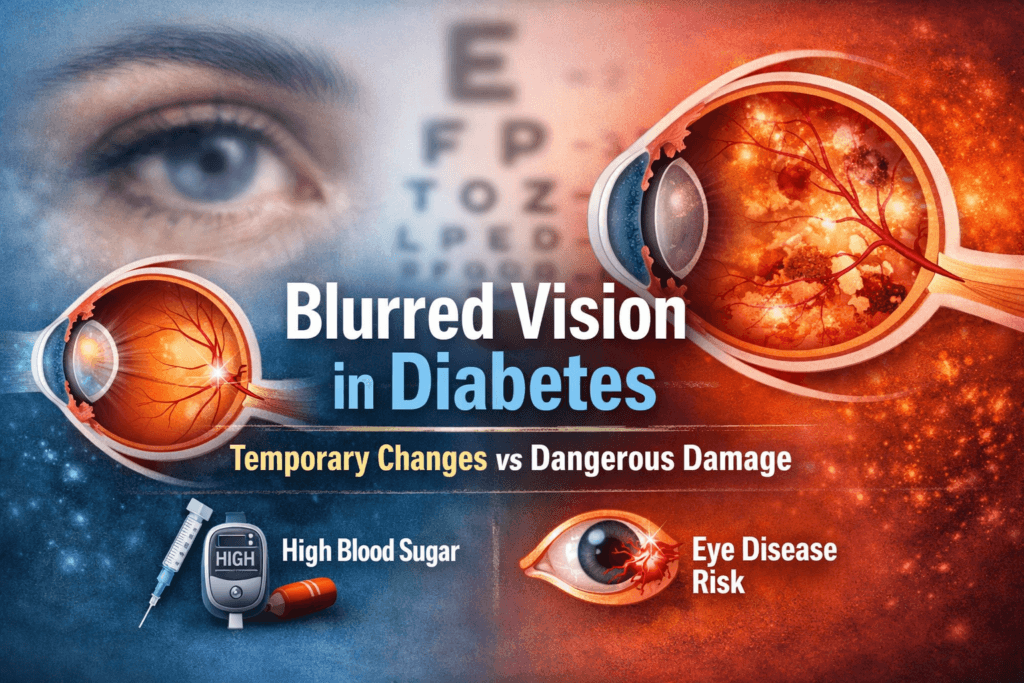
Blurred vision is one of the most misunderstood and underappreciated symptoms of diabetes, some people shrug it off, assuming it’s temporary or harmless. Others freeze in panic, fearing the worst, permanent vision loss. Both reactions miss the critical truth.
In reality, blurred vision in diabetes can signal two very different processes:
- A temporary, reversible effect caused by fluctuations in blood sugar
- A progressive, structural eye disease that can quietly damage your vision if left untreated
The tricky part? At first, these two feel almost identical, One might improve after a meal or a dose of insulin, while the other creeps along silently, doing permanent damage without pain or warning.
Knowing the difference isn’t optional, it can mean the difference between returning to normal vision and irreversible loss.
In this article, we’ll guide you through:
- Why diabetes affects your vision in the first place
- What causes temporary blurred vision
- How to recognize warning signs of dangerous eye damage
- Practical tips for distinguishing the two
- When to act immediately to protect your eyesight
- Long-term strategies to keep your vision healthy
No fluff, no sugarcoating, just clear explanations, evidence-based insight, and actionable advice so you can protect your most precious sense.
Why Diabetes Affects Vision in the First Place
Vision relies on an incredibly delicate system, where even small disruptions can blur the world around you. Clear sight depends on three essential components:
- Optical clarity: The cornea, lens, and vitreous must remain transparent and properly shaped to focus light accurately onto the retina.
- Healthy blood vessels: Tiny retinal capillaries supply oxygen and nutrients to the retina. Any compromise affects retinal function.
- Accurate nerve signaling: The retina’s photoreceptors must convert light into electrical signals, and the optic nerve must transmit these signals reliably to the brain.
Diabetes threatens all three. Chronic high blood sugar creates a cascade of harmful effects:
- Fluid shifts inside the eye: Excess glucose alters osmotic balance, causing swelling in the lens and retina.
- Microangiopathy: Small blood vessels weaken, leak, or close, reducing oxygen supply.
- Inflammation and oxidative stress: High glucose accelerates free radical formation, which damages delicate eye tissues.
- Nerve dysfunction: Diabetic neuropathy can affect the optic nerve, subtly impairing vision even before structural damage occurs.
The eyes are uniquely vulnerable because retinal vessels are tiny, delicate, and highly metabolically active. Even brief episodes of uncontrolled glucose can trigger changes that affect clarity of vision, sometimes before the individual notices any symptoms.
Temporary Blurred Vision: What’s Actually Happening
The Lens and Glucose Swings
The most common cause of temporary blurred vision in diabetes is not structural damage, it’s rapid fluctuations in blood sugar affecting the lens of the eye.
Here’s what happens:
- When blood glucose rises, excess glucose enters the lens.
- The lens converts glucose into sorbitol, a sugar alcohol.
- Sorbitol draws water into the lens, causing it to swell and subtly change shape.
- When blood glucose falls, the lens releases water and returns to its previous shape.
This constant swelling and shrinking changes the eye’s focusing power, producing a blurred image on the retina.
Key Characteristics of Temporary Blurring
Temporary blurred vision caused by fluctuating glucose typically:
- Appears during periods of poor glucose control
- Fluctuates throughout the day depending on meals, insulin, or medication
- Improves when blood sugar stabilizes
- Usually affects both eyes symmetrically
- Does not cause pain, floaters, or dark spots
Crucially, this type of blurring:
- Does not permanently damage the eye
- Resolves gradually once glucose levels remain stable for several weeks
Common Situations Where Temporary Blurring Occurs
- Newly diagnosed diabetes before blood sugar is controlled
- Rapid correction of very high glucose
- Medication changes, such as starting insulin or new oral agents
- Periods of illness, infection, or stress, which spike blood sugar
- Poor adherence to treatment plans, including diet and exercise
Why Glasses Don’t Always Fix It
During unstable blood sugar, prescriptions are essentially moving targets. Updating your glasses during these periods is often frustrating: the blurred vision may return as glucose fluctuates.
Eye specialists typically recommend waiting 6-8 weeks of stable blood sugar before obtaining a new prescription. This ensures your glasses match your eyes’ true, stable refractive state.
Dangerous Blurred Vision: When Diabetes Damages the Eye
Temporary blurring is uncomfortable but not the real threat. The dangerous form comes from structural damage inside the eye, caused by prolonged high blood sugar.
The primary culprit is diabetic retinopathy, a condition that gradually damages retinal blood vessels. It is the leading cause of preventable blindness in adults worldwide.
How Diabetic Retinopathy Develops
Persistent hyperglycemia damages the retinal microvasculature through several mechanisms:
- Weakening of vessel walls: Chronic high glucose thins capillary walls, making them prone to rupture.
- Microaneurysms: Small balloon-like bulges form along vessels, which may leak fluid or blood.
- Fluid and blood leakage: Leakage causes swelling in the retina, particularly in the macula (diabetic macular edema), directly impairing central vision.
- Reduced oxygen delivery: Damaged vessels fail to supply adequate oxygen, creating retinal ischemia.
In response to ischemia, the retina sometimes grows new, abnormal blood vessels, a process called neovascularization. These vessels are fragile and can rupture, leading to sudden, severe vision loss.
Stages of Diabetic Retinopathy
Diabetic retinopathy progresses through distinct stages, each carrying increasing risk to vision. Understanding these stages helps distinguish temporary blurred vision from sight-threatening changes.
1. Non-Proliferative Diabetic Retinopathy (NPDR)
This is the early stage, often without noticeable symptoms. Many people are unaware anything is happening in their eyes.
Key features include:
- Microaneurysms: Tiny bulges in retinal blood vessels
- Small retinal hemorrhages: Minor bleeding within the retina
- Hard exudates: Lipid deposits from leaking blood vessels
- Mild vision changes: Occasionally subtle blurring
Vision may be intermittently blurry but often resolves temporarily. Early detection is critical because damage at this stage is reversible or manageable.
2. Diabetic Macular Edema (DME)
DME occurs when fluid leaks into the macula, the central part of the retina responsible for sharp, detailed vision. This is when blurred vision becomes persistent and functionally impactful.
Symptoms include:
- Persistent blurred or wavy vision
- Difficulty reading, driving, or recognizing faces
- Dark or empty spots in central vision
DME can develop at any stage of retinopathy and is a leading cause of vision loss in people with diabetes. Early treatment can stabilize or even improve vision.
3. Proliferative Diabetic Retinopathy (PDR)
This is the advanced stage, triggered by severe oxygen deprivation in the retina. In response, the retina grows abnormal new blood vessels (neovascularization), which are fragile and prone to bleeding.
Potential consequences:
- Vitreous hemorrhage: Sudden, severe vision loss due to bleeding into the eye
- Retinal detachment: May require urgent surgery
- Permanent blindness: If untreated, vision loss can be irreversible
PDR is often discovered too late because earlier, asymptomatic stages were ignored. Early detection through regular eye exams is essential to prevent severe outcomes.
How to Tell Temporary Blurring from Dangerous Damage
Temporary Blurred Vision Tends to:
- Fluctuate throughout the day depending on blood sugar
- Improve when glucose stabilizes
- Affect both eyes symmetrically
- Occur without floaters, shadows, or dark spots
- Resolve within weeks once blood sugar is controlled
Dangerous Blurred Vision Often:
- Persists even after blood sugar is stable
- Gradually worsens over time
- May affect one eye more than the other
- Includes floaters, flashes, or dark spots
- Causes distorted, wavy, or missing central vision
If blurred vision does not improve after glucose stabilization, it is not simply a temporary sugar-related effect, prompt evaluation is required.
Red Flags That Require Immediate Eye Evaluation
Seek urgent ophthalmologic care if you experience any of the following:
- Sudden vision loss
- New floaters or cobweb-like shadows
- Flashes of light
- A dark curtain across your field of vision
- Severe eye pain o redness
- Distorted or wavy central vision
These are serious warning signs, not symptoms to watch and wait on. Early intervention can make the difference between saving or losing vision.
Why Good Vision Today Does NOT Mean Healthy Eyes
A dangerous misconception in diabetes is:
“I see fine, so my eyes are fine.”
Early diabetic retinopathy:
- Often causes no pain
- May not affect vision initially
- Progresses silently over years
By the time vision changes become noticeable, structural damage may already be advanced. This is why routine eye exams are critical, even if vision seems normal.
Eye Exam Guidelines for People with Diabetes
- Type 1 Diabetes: Eye exam within 5 years of diagnosis
- Type 2 Diabetes: Eye exam at diagnosis
- Pregnancy with Diabetes: Before conception and during pregnancy
- After Diagnosis: At least once yearly, or more frequently if retinopathy is present
Only a dilated retinal exam can detect early damage that could otherwise go unnoticed.
The Role of Blood Sugar Control
Tight glucose control is the most effective way to prevent or slow diabetic eye disease. Benefits include:
- Reduced risk of developing retinopathy
- Slower progression of existing disease
- Lower likelihood of needing invasive treatments
Even small improvements in glucose control make a meaningful difference. Long-term stability matters far more than short-term perfection.
Other Risk Factors That Accelerate Eye Damage
Vision loss in diabetes is rarely caused by glucose alone. Contributing factors include:
- High blood pressure
- Elevated cholesterol
- Smoking
- Long duration of diabetes
- Kidney disease
- Poor follow-up or missed eye exams
Addressing these factors alongside blood sugar control significantly reduces the risk of severe vision loss.
Treatment Options When Damage Exists
Modern ophthalmology offers several interventions that can preserve or even improve vision if caught early:
- Anti-VEGF injections: Reduce abnormal vessel growth and fluid leakage
- Steroid injections or implants: Control inflammation and swelling
- Laser photocoagulation: Seals leaking vessels and prevents further damage
- Vitrectomy surgery: Removes blood or scar tissue in advanced cases
Early treatment works best. Once structural damage is advanced, treatments are less effective, and vision may be permanently lost.
Can Blurred Vision Be Prevented?
The good news, most diabetes-related vision loss is preventable. Vision complications rarely appear overnight they develop gradually over years of unnoticed changes. The key is proactive, consistent care.
Steps to Protect Your Eyes
- Maintain stable blood glucose:
Keeping your blood sugar within target ranges reduces stress on retinal blood vessels and minimizes temporary lens swelling. Consistency matters more than perfection, small, sustained improvements protect your eyes over the long term. - Schedule regular eye exams:
Early diabetic retinopathy often produces no symptoms. Routine dilated eye exams allow doctors to detect changes before vision is affected, making early intervention possible. - Control blood pressure and cholesterol:
High blood pressure and elevated cholesterol accelerate retinal damage. Managing these factors protects both your heart and your eyes. - Quit smoking:
Smoking worsens vascular damage and slows healing. Stopping significantly lowers your risk of severe eye disease. - Act promptly on abnormalities:
If your ophthalmologist identifies early changes such as microaneurysms, macular swelling, or neovascularization early treatment works best, waiting until symptoms worsen reduces the chance of preserving vision.
Blindness from diabetes is rarely sudden. In most cases, it is the end result of years of missed warning signs. By controlling blood sugar, monitoring your eyes, and managing other health risks, you can prevent most vision loss and keep your eyesight sharp well into the future.
Final Truth: No Reassurance Without Evidence
Blurred vision in diabetes is not a single, uniform symptom. It can mean very different things:
- A temporary lens response to fluctuating blood sugar that may resolve once glucose stabilizes.
- A warning sign of retinal damage, structural changes in the eye that will not reverse on their own.
Ignoring blurred vision because it comes and goes is one of the most common ways people lose sight permanently.
What you must do:
- Stabilize your blood sugar: consistent glucose control is the first line of defense.
- Get regular, dilated eye exams: early detection is the only way to catch silent damage.
- Act promptly on abnormalities: delaying treatment increases the risk of irreversible vision loss.
Vision loss from diabetes is common, but it is not inevitable, with vigilance, proactive care, and timely intervention, you can preserve your eyesight and maintain a clear, healthy view of the world.
🔹 Need Health Clarity?
Get expert advice fast and confidentially. MuseCare Consult doctors are ready to help you understand symptoms, labs, and medications in a session designed just for you.
🔹 Book a ConsultRecommended Post:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- 10 Proven Tips on How to Interpret Hemoglobin A1c Levels Accurately
- Fasting Blood Sugar vs HbA1c vs OGTT: 7 Critical Differences Every Patient Must Know
- 10 Critical Insights Into Frequent Urination and Thirst in Diabetes: The Physiology Behind Classic Symptoms
- Unexplained Weight Loss or Gain in Diabetes: 11 Shocking Reasons It Happens
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- How Blood Sugar Is Regulated in the Body: 10 Key Mechanisms Explained
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


