⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
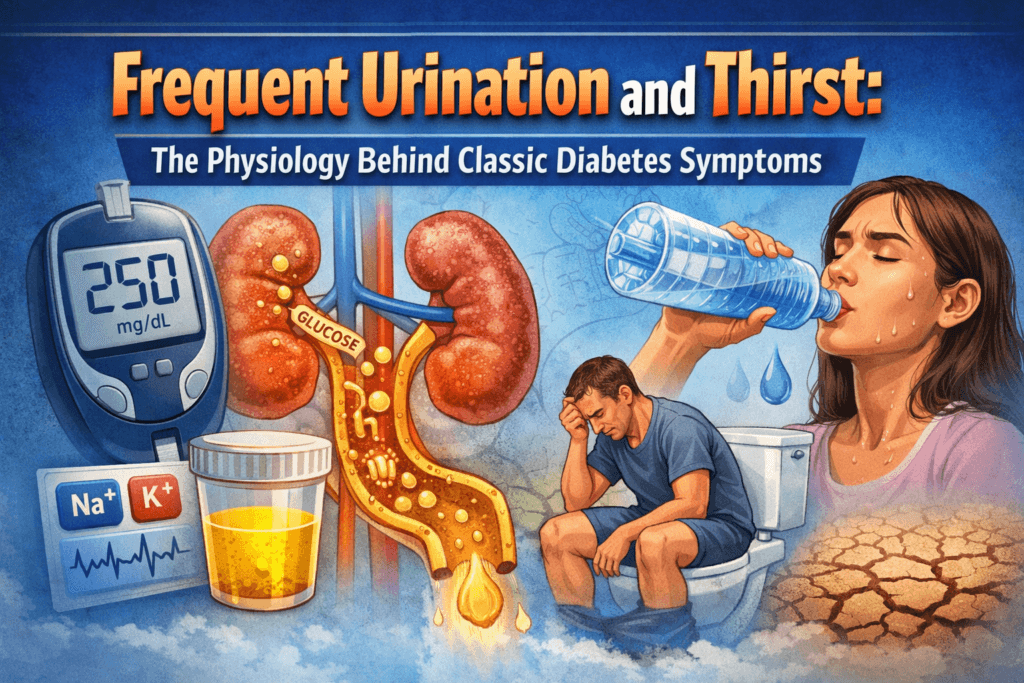
10 Critical Insights Into Frequent Urination and Thirst in Diabetes: The Physiology Behind Classic Symptoms
Frequent urination and unrelenting thirst are often dismissed as everyday annoyances, too much water, hot weather, stress, or simply getting older. Yet in clinical medicine, these two symptoms have long carried far more weight before laboratory diagnostics and modern glucose monitoring existed, physicians relied heavily on excessive urination and thirst as early warning signals of diabetes mellitus. Even today, they remain among the most common reasons individuals first seek medical evaluation before a formal diagnosis is made.
What makes these symptoms dangerous is not their familiarity, but how easily they are misunderstood. Polyuria and polydipsia are not random or harmless bodily reactions. They are precise, predictable responses to persistently elevated blood glucose levels. When glucose rises beyond the body’s ability to regulate it, a cascade of physiological events is triggered, one that places the kidneys at the center of symptom development.
This article breaks down that process step by step, it explains how glucose is normally managed, what changes when insulin is absent or ineffective, and why the kidneys respond in a way that produces frequent urination and intense thirst. Understanding this physiology does more than explain symptoms, it reveals why these signs often mean diabetes has already progressed beyond a silent stage and why early detection matters.
Normal Glucose Regulation: How the System Should Work
Under normal physiological conditions, blood glucose levels are maintained within a remarkably narrow range. After a meal, dietary carbohydrates are digested into glucose, which is absorbed into the bloodstream and causes a predictable rise in blood glucose concentration.
This increase is sensed by pancreatic beta cells located in the islets of Langerhans, prompting the release of insulin. Insulin functions as the body’s primary anabolic hormone, signaling that energy is available. It facilitates the movement of glucose from the bloodstream into insulin-sensitive tissues, particularly skeletal muscle, adipose tissue, and the liver where glucose can be immediately used for energy or stored as glycogen for future needs.
Simultaneously, insulin suppresses hepatic glucose output by inhibiting glycogen breakdown and gluconeogenesis. These coordinated actions work together to prevent excessive postprandial hyperglycemia and restore blood glucose levels toward baseline.
The kidneys play a quieter but equally critical role in glucose homeostasis. As blood passes through the glomeruli, glucose is freely filtered into the renal tubules along with water and electrolytes. In healthy individuals, almost all of this filtered glucose is reclaimed in the proximal tubule through specialized sodium-glucose cotransporters.
Because reabsorption is highly efficient under normal conditions, urine contains little to no glucose. Glucose remains in circulation where it can be utilized by tissues, and water balance is preserved.
This finely tuned system functions effectively as long as two conditions are met, blood glucose levels remain below the renal reabsorption threshold, and insulin secretion and signaling remain intact. When either component fails, the balance is disrupted and the characteristic symptoms of diabetes begin to emerge.
What Goes Wrong in Diabetes
Diabetes disrupts a tightly regulated system designed to maintain stable blood glucose and cellular energy supply. Whether the problem is absolute insulin deficiency as seen in Type 1 diabetes, or insulin resistance with relative insulin deficiency in Type 2 diabetes, the end result is the same, glucose cannot effectively enter insulin-dependent tissues.
As glucose accumulates in the bloodstream, hyperglycemia develops. Paradoxically, despite an excess of circulating glucose, cells are unable to access it and are left in a state of functional energy deprivation. The body interprets this as starvation and responds by increasing hunger, breaking down fat and muscle for fuel, and activating counter-regulatory hormones that further raise blood glucose levels.
At the same time, the kidneys, whose role is to filter and regulate blood contents are exposed to glucose concentrations far beyond physiological norms. This renal overload marks the beginning of the classic urinary symptoms of diabetes.
Renal Glucose Handling and the Renal Threshold
Under normal conditions, the kidneys filter approximately 180 liters of plasma per day, and this filtrate contains glucose. In healthy individuals, nearly all filtered glucose is reclaimed in the proximal tubules through sodium-glucose cotransporters, primarily SGLT2.
These transporters, however, have a finite capacity. When blood glucose levels rise beyond a critical concentration known as the renal threshold for glucose, the transporters become saturated. Once this threshold is exceeded, glucose can no longer be fully reabsorbed and begins to appear in the urine, a phenomenon known as glycosuria.
Glycosuria is not a harmless laboratory finding. The presence of glucose within the renal tubules fundamentally disrupts normal water and electrolyte handling, setting the stage for significant fluid loss.
Osmotic Diuresis: The Core Mechanism Behind Frequent Urination
Glucose is an osmotically active molecule. When it remains in the tubular fluid, it retains water within the nephron, preventing normal reabsorption. This process, osmotic diuresis is the central mechanism responsible for frequent urination in diabetes.
As urinary glucose concentration rises, so does urine volume. The consequences include:
- Increased total urine output
- Frequent daytime urination
- Nocturia, often requiring multiple awakenings at night
Crucially, osmotic diuresis is not under voluntary control, reducing fluid intake does not stop urine production. As long as hyperglycemia persists, glucose will continue to pull water into the urine.
Prolonged osmotic diuresis also leads to the loss of electrolytes, particularly sodium and potassium. This contributes to symptoms such as fatigue, muscle weakness, lightheadedness, and impaired concentration.
Why Thirst Follows: The Physiology of Polydipsia
Persistent water loss inevitably leads to dehydration. As circulating volume declines and plasma osmolality rises, specialized osmoreceptors in the hypothalamus detect the imbalance and activate the brain’s thirst center.
The resulting thirst is intense and unrelenting, it is not relieved by small or moderate fluid intake and often persists even after drinking large volumes of water.
Dehydration also triggers the release of antidiuretic hormone (ADH), which normally signals the kidneys to conserve water. However, in the presence of glucose-driven osmotic diuresis, ADH is largely ineffective, the kidneys simply cannot reabsorb sufficient water while glucose remains trapped in the tubules.
This creates a self-perpetuating cycle:
- Elevated blood glucose leads to glycosuria
- Glycosuria causes osmotic diuresis
- Excessive urination results in dehydration
- Dehydration triggers intense thirst
- Fluid intake fails to halt urination as long as hyperglycemia persists
Only correction of blood glucose levels can interrupt this cycle.
Why These Symptoms Can Appear Suddenly
In Type 1 diabetes, frequent urination and excessive thirst often develop rapidly, over days to weeks. This reflects the abrupt onset of insulin deficiency, which causes a swift rise in blood glucose and early saturation of renal glucose transporters.
In Type 2 diabetes, the process is usually slower, Insulin resistance may be present for years before blood glucose levels rise high enough to exceed the renal threshold. When that threshold is finally crossed, symptoms may seem to appear suddenly, even though metabolic dysfunction has been progressing silently for a long time.
This delayed symptom onset is a major reason Type 2 diabetes is frequently diagnosed late, sometimes only after dehydration, infections, or vascular complications have already developed.
Frequent urination and excessive thirst are not coincidental symptoms, they are the direct physiological consequences of uncontrolled hyperglycemia overwhelming renal glucose handling. When these signs appear, they signal that glucose regulation has already failed and that immediate evaluation and intervention are necessary, not optional.
Differences Between Type 1 and Type 2 Diabetes
While the underlying mechanism of frequent urination and thirst is similar in both types, there are important distinctions:
Type 1 Diabetes
- Absolute insulin deficiency
- Rapid onset of symptoms
- Severe hyperglycemia
- Higher risk of dehydration and diabetic ketoacidosis
Type 2 Diabetes
- Insulin resistance with relative insulin deficiency
- Gradual onset
- Symptoms may be milder initially
- Often overlooked or attributed to aging or lifestyle factors
Regardless of type, the presence of polyuria and polydipsia indicates that blood glucose has exceeded safe levels.
Why Drinking More Water Doesn’t Fix the Problem
When excessive thirst develops, many people instinctively respond by drinking more water. While hydration is essential for basic physiological function, it does not correct the root cause of the problem in diabetes.
In uncontrolled hyperglycemia, blood glucose levels rise above the kidney’s reabsorption threshold. Once this threshold is exceeded, glucose spills into the urine because glucose is osmotically active, it drags water along with it, a process known as osmotic diuresis. The result is persistent, high-volume urine output.
Drinking more water may temporarily relieve the sensation of dryness or thirst, but it does nothing to stop glucose loss in the urine. As long as blood glucose remains elevated, the kidneys will continue to excrete both glucose and water, perpetuating dehydration.
In more severe cases, excessive water intake without correcting hyperglycemia can actually be harmful. Dilution of electrolytes, particularly sodium and potassium can worsen weakness, dizziness, confusion, and in extreme cases, precipitate neurological complications.
True resolution requires glycemic control, not just fluid replacement. This may involve insulin therapy, oral glucose-lowering medications, structured dietary changes, increased physical activity, or a combination tailored to the individual.
Clinical Importance: When These Symptoms Should Not Be Ignored
Frequent urination (polyuria) and excessive thirst (polydipsia) are not normal variations of hydration behavior. When they are persistent, progressive, or unexplained, they represent important clinical warning signs.
Failure to recognize and investigate these symptoms can lead to serious complications, including:
- Severe dehydration, due to ongoing fluid losses
- Electrolyte imbalances, affecting cardiac, muscular, and neurological function
- Diabetic ketoacidosis (DKA), particularly in Type 1 diabetes, characterized by acidosis, ketone production, and rapid clinical deterioration
- Hyperosmolar hyperglycemic state (HHS), more common in Type 2 diabetes, marked by extreme hyperglycemia, profound dehydration, and high mortality risk
Early recognition allows for prompt diagnosis and intervention, dramatically reducing the likelihood of these life-threatening outcomes.
Why These Symptoms Often Occur Together
Polyuria and polydipsia rarely appear in isolation, they are typically part of a broader metabolic disturbance caused by insulin deficiency or insulin resistance.
Common accompanying symptoms include:
- Fatigue, due to impaired glucose uptake at the cellular level despite high blood glucose
- Unexplained weight loss, resulting from breakdown of fat and muscle for energy
- Blurred vision, caused by osmotic shifts affecting the lens of the eye
- Dry skin and dry mouth, reflecting ongoing fluid loss
Together, these findings form a classic clinical pattern that should immediately raise suspicion for diabetes and prompt further evaluation.
The Role of Modern Diabetes Medications
Interestingly, modern diabetes pharmacology deliberately harnesses this same renal mechanism. Sodium-glucose cotransporter-2 (SGLT2) inhibitors lower blood glucose by blocking glucose reabsorption in the kidneys, increasing urinary glucose excretion.
While this approach is effective and provides cardiovascular and renal benefits, it also explains common side effects such as increased urination, thirst, and a higher risk of dehydration if fluid intake is inadequate.
This therapeutic strategy underscores an important physiological principle, renal glucose handling has a powerful influence on fluid balance. In uncontrolled diabetes, this mechanism operates unchecked, producing the prominent urinary and thirst symptoms seen in clinical practice.
Conclusion
Frequent urination and excessive thirst are neither random nor benign complaints. They are the direct, predictable physiological outcomes of sustained hyperglycemia, occurring when blood glucose levels overwhelm the kidneys’ capacity to reclaim glucose. Once that threshold is crossed, osmotic diuresis takes over, glucose pulls water with it into the urine, driving ongoing fluid loss and triggering an intense, compensatory thirst response.
This mechanism reveals an uncomfortable truth, by the time these symptoms appear, diabetes is already placing significant metabolic strain on the body. They are not early inconveniences to be normalized or managed with more water, they are warning signals that fundamental glucose regulation has failed.
Understanding the physiology behind these classic signs reframes their importance. It prompts individuals to seek timely testing, equips clinicians to intervene decisively, and helps patients grasp why blood glucose control matters, not only to prevent distant complications, but to restore immediate physiological balance. Early recognition is not optional. It preserves metabolic stability, limits tissue damage, and, in many cases, saves lives.
🩺 Talk to a Health Expert Today
Personalized advice matters. Connect with licensed doctors at MuseCare Consult to review your symptoms, labs, or medications in a private, convenient session.
👉 Schedule Your ConsultRecommended Blog Post:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- How Blood Sugar Is Regulated in the Body: 10 Key Mechanisms Explained
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- Early Warning Signs of Diabetes Most People Ignore: 10 Subtle Symptoms You Must Know
- Unexplained Weight Loss or Gain in Diabetes: 11 Shocking Reasons It Happens
- 12 Powerful Early Signs of Insulin Resistance You Should Watch and How to Fix Them
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


