⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission at no extra cost to you, if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
Unexplained Weight Loss or Gain in Diabetes: 11 Shocking Reasons It Happens
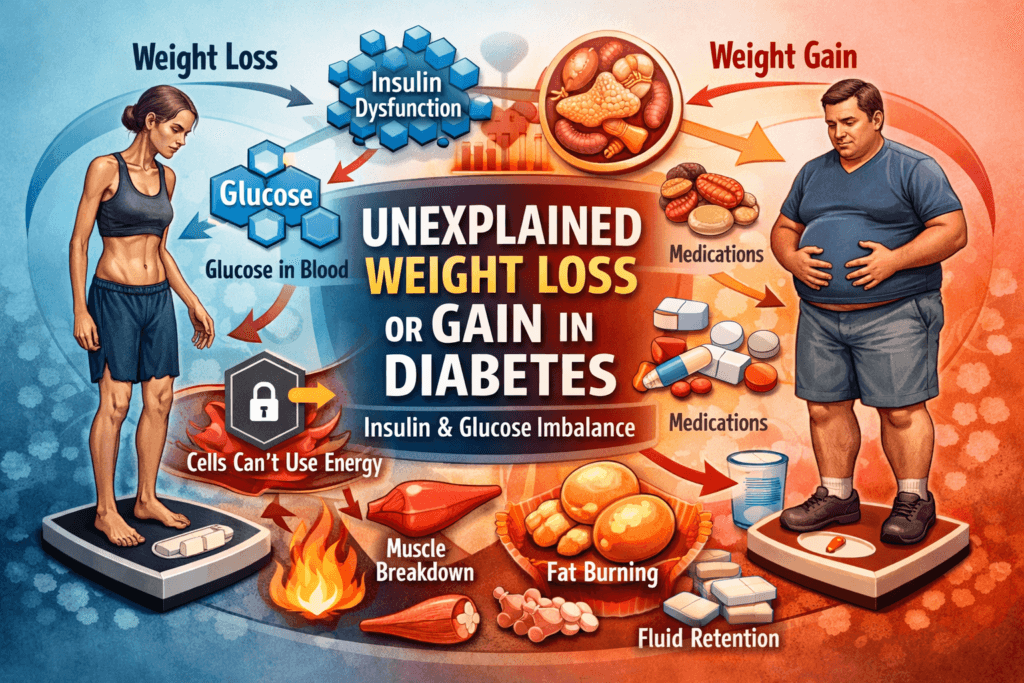
Weight change is often the first visible clue that something deeper has gone wrong but it’s also one of the most misunderstood signals in diabetes. People expect diabetes to look a certain way, weight gain, overeating, “too much sugar”. Reality is messier, some individuals lose weight rapidly before they’re ever diagnosed, others gain weight shortly after starting treatment. Many swing between loss and gain, unable to explain why their body no longer behaves predictably.This isn’t coincidence, and it isn’t personal failure.
When diabetes develops, the body’s energy system breaks down, glucose may be abundant in the bloodstream, yet inaccessible to the cells that need it, hormones that normally coordinate storage, release, and use of energy stop working in sync. As a result, the body may start wasting calories through urine, breaking down muscle for fuel, hoarding fat despite low energy levels, or doing all of these at once. What shows up on the scale is simply the outward expression of that internal disorder.
This is why weight changes in diabetes often feel confusing or unfair, you may be eating the same way yet losing weight or eating less and still gaining. You may do everything right and watch your body move in the opposite direction. The scale becomes a source of anxiety because it’s reflecting metabolic chaos not discipline, effort, or intention.
To make sense of unexplained weight loss or gain in diabetes, you have to stop looking at calories alone and start looking at physiology. Once you understand how insulin dysfunction, glucose mismanagement, muscle breakdown, and fat storage interact, the pattern becomes clear.
The Core Problem: Energy Is Present but Not Accessible
At its core, diabetes is not simply a condition of too much sugar. That framing is misleading and incomplete, diabetes is fundamentally a disorder of energy mismanagement.
In a healthy system, glucose in the bloodstream represents usable energy. Insulin acts as the key that allows this energy to move from the blood into cells, where it can be burned for fuel or stored for later use. In diabetes, that process breaks down.
- Glucose is abundant in the blood
- Cells cannot access it efficiently
- The body behaves as though it is starving, despite having plenty of fuel available
This mismatch, energy everywhere, but unavailable where it’s needed sets off a cascade of survival responses, hormones shift, tissues adapt and metabolism turns destructive. Every unexplained weight change in diabetes flows directly from this single problem, from here, everything else follows.
Why Uncontrolled Diabetes Causes Weight Loss
Unintentional weight loss is especially common in undiagnosed diabetes or in cases where blood glucose remains poorly controlled. It is most dramatic in Type 1 diabetes, but it also occurs in advanced or insulin-deficient Type 2 diabetes.
This weight loss is not healthy, intentional, or desirable, it is the visible result of the body failing to access its primary energy source.
1. Glucose Is Lost Through Urine (Calorie Wasting)
Under normal circumstances, the kidneys filter glucose out of the blood and then reabsorb nearly all of it back into circulation. Glucose is too valuable to waste. However, when blood glucose rises above the renal threshold, approximately 180 mg/dL (10 mmol/L)-the kidneys can no longer keep up.
- Glucose spills into the urine
- Each gram of glucose lost represents 4 calories
- Persistent glycosuria leads to continuous calorie loss
This means you can eat more food and still lose weight, because a portion of your energy intake never reaches your tissues. It is quite literally flushed away. This is not fat loss driven by improved metabolism, it is metabolic leakage, energy escaping the body because insulin is not doing its job.
2. Insulin Deficiency Forces the Body to Burn Muscle and Fat
Insulin is often reduced to a blood sugar hormone, but that description misses its most important role. Insulin is the body’s primary anabolic hormone, it tells tissues to build, store, and preserve.
When insulin is absent or ineffective:
- Muscle protein is broken down into amino acids
- Fat tissue is broken down into free fatty acids
- The liver converts these substrates into glucose and ketones to keep vital organs alive
This internal recycling is a survival mechanism, not a healthy adaptation.
The consequences are predictable:
- Progressive muscle wasting
- Loss of fat mass
- Overall weight reduction
The body is not slimming down, it is breaking itself down to compensate for its inability to use glucose.
3. Ketone Production Accelerates Fat Loss (Especially in Type 1 Diabetes)
In severe insulin deficiency, most notably in untreated Type 1 diabetes, fat breakdown becomes extreme.
- Fat is rapidly mobilized from adipose tissue
- The liver converts large amounts of fat into ketone bodies
- Energy production shifts into emergency mode
As ketone production increases, weight loss accelerates. This is why dramatic, rapid weight loss is often one of the earliest signs of Type 1 diabetes. Importantly, this process is dangerous, excess ketones can acidify the blood, leading to diabetic ketoacidosis (DKA).
Weight loss in this context is not a metabolic success, it is a medical warning sign, indicating that the body is operating without its primary regulatory hormone.
4. Dehydration Creates False Weight Loss
Not all early weight loss in diabetes comes from fat or muscle. A significant portion can be explained by fluid loss.
High blood glucose causes osmotic diuresis:
- Glucose pulls water into the urine
- Urine volume increases dramatically
- Electrolytes and fluids are lost
This leads to dehydration, which can reduce body weight quickly. When blood glucose is later controlled and hydration is restored, some of that weight returns. Many people interpret this as sudden fat gain, but that’s incorrect. In most cases, it is simply replenished water, not stored fat. Understanding this distinction matters otherwise, normal recovery can feel like failure.
Why Diabetes Can Also Cause Weight Gain
Now let’s address the opposite side of the spectrum, weight gain. This is the part that confuses people the most, because it seems to contradict everything they’ve been told. How can a disease associated with high blood sugar and poor energy use also cause fat accumulation?
The answer, again, lies in hormones—not willpower.
1. Insulin Promotes Fat Storage
Insulin has one dominant biological instruction, which is to store energy.
When insulin is present, especially in high or prolonged amounts, it signals the body to move nutrients out of the bloodstream and into storage sites primarily fat tissue.
When insulin levels are elevated:
- Glucose is driven into fat cells
- Fat breakdown (lipolysis) is actively suppressed
- New fat production (lipogenesis) increases
In Type 2 diabetes and insulin resistance, insulin levels are often chronically high. The pancreas produces more and more insulin in an attempt to overcome resistance, and this persistent elevation strongly favors fat storage.
The result is not just general weight gain, but preferential accumulation of visceral fat, the deep abdominal fat that worsens insulin resistance and cardiovascular risk.
This process is not driven by overeating alone, it is the result of a hormonal bias toward storage, even when calorie intake appears reasonable.
2. Insulin Resistance Traps Fat in Fat Cells
This is one of the most important and least understood paradoxes in diabetes.
In insulin resistance:
- Muscle cells become resistant to insulin and struggle to take up glucose
- Fat cells remain relatively insulin sensitive and continue storing energy
So while muscles are starved of fuel, fat tissue keeps expanding. The consequences are predictable:
- Fat mass increases
- Muscle energy availability drops
- Fatigue worsens
- Hunger signals intensify
This explains why many people with Type 2 diabetes gain weight while feeling tired, weak, and constantly hungry, even without eating excessively. The body is directing energy into storage while depriving the tissues that actually need it.
3. Diabetes Medications Can Cause Weight Gain
This is a critical point, and one many patients are never clearly told, some diabetes treatments cause weight gain by design. These medications often improve blood glucose control, but they do so by shifting how and where energy is stored.
Insulin therapy
- Stops glucose loss through the urine
- Restores glucose uptake into tissues
- Eliminates calorie wasting
If calorie intake is not adjusted, weight gain can follow. In many cases, this is restorative weight, the return of energy that was previously being lost. After uncontrolled diabetes, some weight regain is expected and physiologically appropriate.
Sulfonylureas (e.g glibenclamide)
- Stimulate insulin release regardless of glucose needs
- Increase fat storage
- Raise the risk of hypoglycemia
Because low blood sugar triggers hunger, people often eat more to prevent or treat symptoms. Weight gain here is driven by medication effects, not lack of control.
Thiazolidinediones (TZDs)
- Improve insulin sensitivity at the cellular level
- Increase fat mass and cause fluid retention
The number on the scale may rise even as glucose control improves. This weight gain reflects changes in fat distribution and water balance not personal failure. In all these cases, weight gain is a pharmacologic effect, not a behavioral one.
4. Overcorrection After Diagnosis
After a diabetes diagnosis, behavior often shifts in subtle but important ways.
Many people:
- Eat preemptively to avoid low blood sugar
- Reduce physical activity out of fear of hypoglycemia
- Over-treat mild lows with excessive calories
Over time, this leads to slow, steady weight gain that feels inevitable and frustrating. It isn’t inevitable but correcting it requires understanding physiology and medication effects, not blame or restriction.
Why Some People Swing Between Weight Loss and Gain
Weight fluctuation in diabetes almost always reflects unstable metabolic control, not inconsistent discipline.
Common contributors include:
- Irregular medication timing or dosing
- Variable insulin absorption
- Recurrent cycles of high and low blood sugar
- Alternating dehydration and rehydration
Each swing on the scale represents shifting internal conditions. The body is reacting to instability, not responding to effort.
Type 1 vs Type 2: Different Mechanisms, Same Outcome
Although the pathways differ, both major types of diabetes disrupt energy balance and body weight.
Type 1 Diabetes
- Absolute insulin deficiency
- Rapid, often dramatic weight loss before diagnosis
- Weight gain after starting insulin is common, expected, and often healthy
Type 2 Diabetes
- Insulin resistance with relative insulin deficiency
- Weight gain typically precedes diagnosis
- Weight loss may occur later as insulin production declines
Different starting points, same underlying issue: impaired energy regulation.
The Role of Muscle: The Missing Conversation
Most discussions about weight focus entirely on fat, but muscle is the largest glucose-using tissue in the body. Ignoring it leads to misunderstanding.
In diabetes:
- Muscle insulin resistance reduces glucose uptake
- Muscle loss further worsens insulin resistance
- Fat gradually replaces muscle, a process known as sarcopenic obesity
This explains why:
- Body weight may remain stable
- Body composition worsens
- Metabolic health continues to decline
The scale may not move, but risk increases. This is why weight alone is a poor marker of metabolic health. Muscle preservation matters, and losing it quietly undermines glucose control.
When diabetes causes weight gain, it is not because the body is lazy or undisciplined, it is because insulin signaling, medication effects, and tissue-specific resistance are pushing energy into storage. Until those forces are addressed, the scale will continue to feel like it’s working against you even when effort is high.
Why Eat Less, Move More Fails in Diabetes
The advice to simply eat less and move more sounds logical but in diabetes, it often fails spectacularly not because people aren’t trying, but because this approach ignores physiology.
When insulin levels are high or insulin resistance is severe:
- Fat burning is actively suppressed
- Hunger signals intensify as cells remain energy-deprived
- Energy levels drop, making sustained activity harder
Under these conditions, reducing calories further doesn’t fix the problem, it often worsens it. The body responds by conserving energy, increasing appetite hormones, and clinging more tightly to stored fat. You end up fighting biology with willpower and biology usually wins.
This is why many people with diabetes feel trapped in a cycle of restriction, fatigue, and rebound weight gain. Sustainable weight regulation in diabetes requires a different focus:
- Improving insulin sensitivity so cells can actually use glucose
- Stabilizing blood sugar to prevent hormonal swings
- Preserving muscle mass, the body’s primary glucose-using tissue
Without these foundations, any weight loss is temporary and often comes at the cost of muscle and metabolic health.
When Weight Change Is a Medical Warning Sign
Not all weight changes are benign, and some should never be ignored.
Red flags include:
- Rapid, unexplained weight loss
- Weight loss accompanied by fatigue, thirst, or frequent urination
- Weight gain with swelling, shortness of breath, or rapid fluid accumulation
- Progressive muscle loss despite stable body weight
These patterns may indicate:
- Poor or deteriorating glycemic control
- Adverse medication effects
- Kidney involvement causing fluid retention
- Heart strain or early heart failure
In diabetes, weight change is not just a cosmetic issue, it is clinical information. Ignoring it can delay diagnosis or treatment of serious complications.
The Real Goal Is Not Weight, It’s Metabolic Control
Focusing solely on the number on the scale leads to frustration and self-blame. Weight is an outcome, not a strategy.
The real goals in diabetes management are:
- Stable blood glucose with minimal highs and lows
- Improved insulin sensitivity across muscle and liver tissue
- Preservation of lean muscle mass
- Reduction of harmful visceral fat
When these are addressed, weight often normalizes on its own, without extreme restriction or constant struggle.
Trying to control weight without fixing metabolism is like mopping the floor while the tap is still running. Turn off the source, and the problem resolves itself.
Final Truth
If there’s one thing to be absolutely clear about, it’s this: unexplained weight loss or weight gain in diabetes has nothing to do with moral failure. It is not about laziness, it is not about weak discipline, it is not about bad character or not trying hard enough.
Those explanations are comforting because they’re simple but they’re wrong. What you see on the scale is the visible consequence of invisible physiology:
- Insulin that cannot signal properly
- Glucose that circulates but cannot be used
- Hormones that push the body toward breakdown or storage at the wrong time
Until those mechanisms are corrected, weight will continue to change regardless of effort, intention, or motivation. You can eat less, move more, and still lose muscle, gain fat, or fluctuate unpredictably, because the system controlling energy is broken.
This is why chasing weight as the primary goal so often ends in frustration. The correct order is non-negotiable:
- Fix glucose regulation
- Restore insulin sensitivity
- Protect muscle
- Stabilize metabolism
Do that, and weight follows naturally, reverse the order, and you spend years fighting your own biology. In diabetes, the truth is simple, even if it’s uncomfortable:
Control the metabolism, and the weight will take care of itself. Not the other way around.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowMust Read:
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- How Blood Sugar Is Regulated in the Body: 10 Key Mechanisms Explained
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- Early Warning Signs of Diabetes Most People Ignore: 10 Subtle Symptoms You Must Know
- 12 Powerful Early Signs of Insulin Resistance You Should Watch and How to Fix Them
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being