⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission — at no extra cost to you — if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
Ulcerative Colitis vs Crohn’s Disease: 11 Key Differences You Must Know
Ulcerative Colitis vs. Crohn’s Disease: Understanding the Key Difference
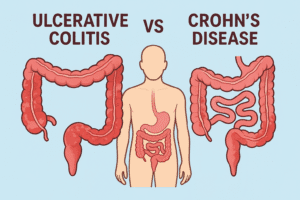
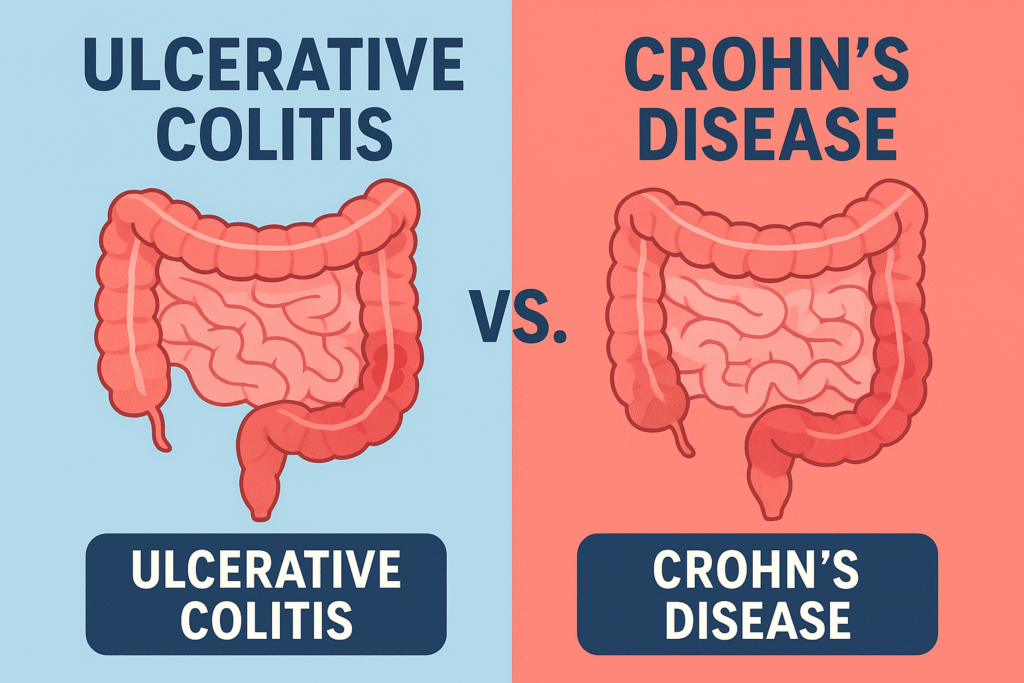
Inflammatory bowel disease refers to a group of long-term conditions that cause persistent inflammation in the gastrointestinal tract. The two most common and well-studied forms are ulcerative colitis and Crohn’s disease.
Although both conditions fall under the IBD umbrella and often share symptoms such as chronic diarrhea, abdominal discomfort, fatigue, and unintentional weight loss, they are distinct diseases with important differences. These differences lie in where they occur in the digestive tract, how deeply the inflammation penetrates the intestinal wall, the pattern of inflammation, potential complications, and their treatment strategies.
Distinguishing between UC and CD is more than a matter of medical classification, it directly influences the choice of therapy, monitoring strategies, and long-term outcomes. Early and accurate diagnosis can help prevent complications, improve symptom control, and preserve quality of life.
In this comprehensive guide, you will learn:
- How ulcerative colitis and crohn’s disease differ in their causes, underlying mechanisms, and areas of the digestive tract affected.
- The key symptoms and signs that can help tell them apart.
- Diagnostic tools doctors use to confirm the condition and assess its severity.
- Treatment approaches, from medication to surgery, and how they vary between UC and CD.
- Lifestyle and dietary strategies that support symptom control and gut health.
- The long-term outlook and ways to maintain remission.
Whether you are a patient, caregiver, or health professional, understanding the differences between ulcerative colitis and Crohn’s disease is essential for informed decision-making and better disease management.
Overview of Ulcerative Colitis and Crohn’s Disease
Ulcerative Colitis (UC)
Ulcerative colitis is a chronic inflammatory bowel disease that affects only the colon (large intestine). The inflammation always starts in the rectum and then extends upward in a continuous pattern toward other parts of the colon. It never affects the small intestine except for a rare backwash ileitis in severe cases.
- Inflammation Pattern: Continuous, no healthy segments between diseased areas.
- Depth of Inflammation: Limited to the mucosa and submucosa (the innermost lining and just beneath it), which explains why complications like strictures and fistulas are rare compared to Crohn’s disease.
- Onset Age: Most people are diagnosed between 15 and 30 years old, with a smaller second peak between 50 and 70 years.
- Disease Course: Tends to follow a pattern of flares and remissions; in some cases, the disease becomes more extensive over time.
Crohn’s Disease (CD)
Crohn’s disease is another form of IBD but can affect any part of the gastrointestinal tract from the mouth to the anus, although the terminal ileum (last part of the small intestine) and the start of the colon are most frequently involved.
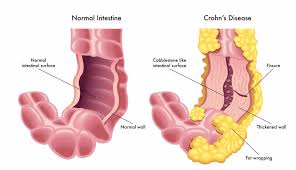
- Inflammation Pattern: Patchy, with “skip lesions” areas of diseased bowel interspersed with normal segments.
- Depth of Inflammation: Transmural: inflammation extends through the entire thickness of the bowel wall, which can lead to complications like strictures, fistulas, and abscesses.
- Onset Age: Commonly diagnosed between 15 and 35 years, though it can develop at any age.
- Disease Course: Often more aggressive than UC, with a higher likelihood of complications and surgery.
Causes and Risk Factors
Although neither ulcerative colitis nor Crohn’s disease has a single known cause, researchers believe they result from a complex interplay of factors, including genetics, immune system dysfunction, environmental triggers, and gut microbiome changes.
Factor | Ulcerative Colitis | Crohn’s Disease |
Genetics | Weaker genetic association; some links to specific HLA genes, especially in extensive disease. | Stronger hereditary influence; NOD2/CARD15 and other gene variants increase susceptibility. |
Immune Response | Abnormal immune reaction that targets the lining of the colon, leading to chronic mucosal inflammation. | Overactive immune system attacking all layers of the bowel wall, and potentially any GI segment. |
Smoking | Surprisingly protective, smokers have a lower risk of UC, but quitting smoking can sometimes trigger onset in susceptible individuals. | Harmful, smoking increases risk, worsens symptoms, and accelerates complications. |
Diet | Diet high in saturated fats, processed foods, and low in fiber may contribute to flares; however, diet alone does not cause UC. | Similar associations; high refined sugar and low-fiber intake linked to increased risk and flare severity. |
Microbiome | Lower diversity and imbalance in gut bacteria (dysbiosis) observed in patients. | Also linked to dysbiosis, but with more profound alterations in bacterial populations. |
Environmental Factors | Higher incidence in developed countries, urban areas, and colder climates, possibly related to hygiene, diet, and antibiotic exposure. | Similar geographic trends, suggesting shared environmental triggers. |
3. Key Symptoms
While ulcerative colitis and Crohn’s disease share many overlapping symptoms due to their inflammatory nature, there are subtle but important differences that can guide both patients and clinicians toward the right diagnosis.
Shared Symptoms
Both UC and CD can present with:
- Chronic diarrhea, often lasting weeks or months, sometimes with mucus or blood.
- Abdominal pain, ranging from mild cramping to severe, disabling pain.
- Fatigue, due to inflammation, poor nutrient absorption, and anemia.
- Weight loss, often a result of reduced appetite, malabsorption, and increased caloric needs from inflammation.
- Blood in stool, caused by intestinal ulceration, more frequent in UC but can occur in CD.
- Loss of appetite, driven by nausea, discomfort, and inflammatory signals from the gut.
Ulcerative Colitis: Specific Symptoms
In UC, the inflammation is limited to the colon and typically starts in the rectum, so symptoms tend to be localized and predictable.
- Bloody diarrhea, the hallmark symptom, often accompanied by mucus; tends to be more severe and persistent compared to CD.
- Urgency to defecate, a sudden, strong need to pass stool, sometimes resulting in incontinence.
- Tenesmus, a constant feeling of needing to pass stool, even when the bowel is empty.
- Lower left abdominal pain, correlates with the descending and sigmoid colon location of inflammation.

Crohn’s Disease: Specific Symptoms
CD can affect any part of the digestive tract and all layers of the bowel wall, leading to a more variable set of symptoms.
- Diarrhea (± blood): may be watery, greasy, or foul-smelling if the small intestine is affected.
- Lower right abdominal pain: often linked to inflammation of the terminal ileum.
- Mouth ulcers: small, painful sores inside the mouth, often during flares.
- Perianal disease: including skin tags, abscesses, and fistulas, due to deep tissue inflammation.
- Bloating and cramping: caused by strictures or partial intestinal blockage.
Symptom Comparison Table
Symptom | Ulcerative Colitis | Crohn’s Disease |
Diarrhea | Always present, often bloody | Often present, blood less common |
Blood in stool | Very common | Occasional |
Abdominal pain location | Lower left abdomen | Lower right abdomen |
Urgency/Tenesmus | Common | Rare |
Mouth ulcers | Rare | Common |
Perianal disease | Rare | Common |
Weight loss | Moderate | Common, often more severe |
Differences in Disease Location and Spread
A defining difference between UC and CD is where the inflammation occurs and how it spreads through the GI tract.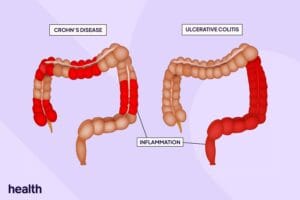
Ulcerative Colitis
- Location: Always starts in the rectum (proctitis) and may extend continuously upward through the colon (left-sided colitis or pancolitis).
- Spread Pattern: Continuous, no normal tissue between inflamed areas.
- Layers Affected: Mucosa and submucosa only: which limits certain complications but increases risk for bleeding.
- Rectal Involvement: Always involved.
- Small Intestine Involvement: Very rare; when present, usually due to backwash ileitis in severe pancolitis.
Crohn’s Disease
- Location: Can occur anywhere from the mouth to the anus, but most commonly affects the terminal ileum and proximal colon.
- Spread Pattern: Patchy inflamed segments separated by areas of normal bowel (“skip lesions”).
- Layers Affected: Transmural, inflammation extends through the entire bowel wall, causing deep ulcers, strictures, and fistulas.
- Rectal Involvement: May be spared.
- Small Intestine Involvement: Common, especially in the terminal ileum, leading to malabsorption of nutrients like vitamin B12 and bile salts.
Location and Spread Comparison Table
Feature | Ulcerative Colitis | Crohn’s Disease |
Location | Colon and rectum only | Anywhere in GI tract |
Pattern | Continuous inflammation from rectum upward | Patchy inflammation (“skip lesions”) |
Layers Affected | Mucosa and submucosa | All layers (transmural) |
Rectal Involvement | Always involved | May be spared |
Small Intestine Involvement | Rare | Common (esp. terminal ileum) |
Extraintestinal Manifestations
Inflammatory bowel disease doesn’t just affect the gut, it can trigger systemic inflammation that impacts other organs and systems. These extraintestinal manifestations (EIMs) may appear before, during, or after intestinal symptoms and can sometimes be more disabling than the bowel disease itself.
Common in Both UC and CD
- Joint involvement (arthritis): the most common EIM, affecting large joints (knees, hips, ankles). It can be peripheral arthritis (linked to disease activity) or ankylosing spondylitis (independent of gut inflammation).
- Eye inflammation
- Uveitis: Inflammation of the middle layer of the eye, causing pain, redness, blurred vision.
- Episcleritis: Milder inflammation of the eye surface, often flaring with intestinal symptoms.
- Uveitis: Inflammation of the middle layer of the eye, causing pain, redness, blurred vision.
- Skin conditions
- Erythema nodosum: Painful, red nodules (usually on shins).
- Pyoderma gangrenosum: Large, painful ulcers, more severe and harder to treat.
- Erythema nodosum: Painful, red nodules (usually on shins).
- Liver and bile duct disease
- Primary sclerosing cholangitis (PSC): Progressive inflammation and scarring of bile ducts; far more common in UC than CD.
- Primary sclerosing cholangitis (PSC): Progressive inflammation and scarring of bile ducts; far more common in UC than CD.
Less Common but Significant
- Kidney stones (more frequent in CD due to malabsorption of oxalate).
- Gallstones (especially in CD with ileal involvement).
- Blood clotting disorders (increased risk of deep vein thrombosis and pulmonary embolism).
Complications
The risk and type of complications vary greatly between UC and CD because of their different inflammation patterns and depths.
Complication | Ulcerative Colitis | Crohn’s Disease |
Colon Cancer | Risk rises with the duration (especially after 8-10 years) and extent of inflammation; regular colonoscopy recommended. | Increased risk, but generally lower than UC unless the colon is extensively involved. |
Strictures | Rare (inflammation is superficial). | Common due to transmural inflammation causing scarring and narrowing of the bowel. |
Fistulas | Rare. | Common, abnormal connections between bowel segments, bladder, skin, or vagina. |
Toxic Megacolon | Possible and potentially life-threatening; requires urgent treatment. | Rare. |
Malabsorption | Uncommon since the small intestine is spared. | Common, especially when the small intestine (ileum) is involved, leading to deficiencies in iron, vitamin B12, and fat-soluble vitamins. |
Abscesses | Rare. | More common due to deep ulceration and transmural involvement. |
Diagnosis
Diagnosing UC and CD requires a multifaceted approach combining patient history, physical examination, lab tests, imaging, and endoscopy. No single test can definitively distinguish the two, but the combination of findings helps guide diagnosis.
1. Clinical History & Physical Exam
- Review of symptoms: duration, severity, triggers, and systemic signs.
- Assessment of risk factors: smoking history, family history of IBD, previous infections, medication use.
2. Endoscopic Evaluation
- Colonoscopy, the gold standard for initial diagnosis:
- UC: Continuous inflammation starting in the rectum, friable mucosa, loss of vascular markings, superficial ulcerations.
- CD: Patchy inflammation, cobblestone appearance (due to deep ulcers and swollen tissue), skip lesions, strictures.
- UC: Continuous inflammation starting in the rectum, friable mucosa, loss of vascular markings, superficial ulcerations.
- Upper endoscopy: considered if symptoms suggest upper GI involvement (more common in CD).
3. Histology (Biopsy)
- Multiple tissue samples taken during colonoscopy.
- UC: Inflammation confined to mucosa/submucosa; crypt abscesses may be seen.
- CD: Transmural inflammation, granulomas (present in ~30% of cases), focal crypt irregularities.
- UC: Inflammation confined to mucosa/submucosa; crypt abscesses may be seen.
4. Laboratory Tests
- Blood tests:
- CRP (C-reactive protein) and ESR (erythrocyte sedimentation rate) measure systemic inflammation.
- CBC (complete blood count): checks for anemia and infection.
- Nutrient levels: vitamin B12, folate, iron, and vitamin D (especially in CD).
- CRP (C-reactive protein) and ESR (erythrocyte sedimentation rate) measure systemic inflammation.
- Stool tests:
- Fecal calprotectin: helps differentiate IBD from irritable bowel syndrome (IBS).
- Stool cultures to rule out infectious causes (Salmonella, Shigella, Clostridioides difficile).
- Fecal calprotectin: helps differentiate IBD from irritable bowel syndrome (IBS).
5. Imaging Studies
- CT or MRI enterography: excellent for detecting small bowel involvement in CD, strictures, abscesses, and fistulas.
- Ultrasound: increasingly used for bowel wall thickness assessment (more common in Europe).
- Barium studies: now less common but can highlight strictures and fistulas.
Differentiating UC and CD in Diagnosis
Test/Feature | Ulcerative Colitis | Crohn’s Disease |
Endoscopy | Continuous inflammation from rectum | Patchy skip lesions |
Depth of inflammation | Mucosal/submucosal | Transmural |
Granulomas on biopsy | Rare | Present in ~30% |
Small bowel imaging | Usually normal | Often abnormal (ileum, jejunum) |
Treatment Approaches
Treatment for ulcerative colitis and Crohn’s disease focuses on controlling inflammation, relieving symptoms, and preventing flare-ups. While the general goal is similar, the approach differs based on the nature of each condition.
Ulcerative Colitis
For mild to moderate UC, aminosalicylates (5-ASA) such as mesalamine are often the first-line treatment. They help reduce inflammation in the colon lining and are effective for maintaining remission.
During flare-ups, corticosteroids may be prescribed to quickly reduce inflammation, but because of their side effects, they are used only for short-term control.
If symptoms return whenever steroids are tapered, immunomodulators like azathioprine or 6-mercaptopurine may be added to keep the disease under control.
For patients with more severe or treatment-resistant disease, biologic therapies are available. These include anti-TNF agents like infliximab and adalimumab, as well as anti-integrin drugs like vedolizumab, which target specific parts of the immune system.
In cases where medications fail or complications arise, surgery specifically a colectomy can be curative since UC is limited to the colon.
Crohn’s Disease
Because Crohn’s disease often affects deeper layers of the bowel and can involve any part of the gastrointestinal tract, the treatment approach is generally more aggressive from the start.
Corticosteroids are used for inducing remission during flare-ups, but long-term use is avoided due to side effects.
Immunomodulators and biologics are often introduced earlier in Crohn’s disease compared to UC, as the condition tends to be more aggressive and prone to complications.
Antibiotics like metronidazole or ciprofloxacin may be used when there are infections related to abscesses, fistulas, or perianal disease.
While surgery can be necessary to manage complications such as strictures, perforations, or abscesses, it is not curative. The disease often recurs in other parts of the digestive tract after surgical removal of affected segments.
Diet and Lifestyle Management
Diet and lifestyle adjustments are important complements to medical treatment, though they cannot replace medications. Both UC and CD patients benefit from eating smaller, more frequent meals instead of large portions, which can reduce digestive stress.
Staying well-hydrated is essential, especially during flare-ups when diarrhea is frequent.
Many people find it helpful to avoid trigger foods that worsen symptoms, such as spicy dishes, high-fat meals, caffeine, alcohol, and, during flares, high-fiber foods that can irritate the bowel.
Stress management plays a significant role in preventing flare-ups. Techniques like yoga, meditation, deep breathing exercises, or even gentle physical activity can help.
For people with Crohn’s disease, quitting smoking is particularly important, as smoking is linked to more severe disease and higher relapse rates.
Prognosis
Both UC and CD are chronic conditions, meaning they require long-term management. However, their outlooks differ.
Ulcerative colitis can often be managed effectively with medication, and in cases where it becomes unresponsive to treatment, surgery to remove the colon can be curative.
Crohn’s disease, on the other hand, tends to be progressive. While surgery can provide relief from complications, it does not cure the disease, and inflammation can return in other areas of the digestive tract. With modern medications, many patients can still achieve long periods of remission and maintain a good quality of life.
Conclusion
Although ulcerative colitis and Crohn’s disease both fall under the umbrella of inflammatory bowel disease, they are far from identical. Their differences in location, depth, and spread of inflammation shape not only their symptoms, but also their complications, prognosis, and treatment approaches. UC is limited to the colon and rectum, spreads in a continuous pattern, and can be cured with surgery. Crohn’s can strike anywhere from mouth to anus, appears in patchy “skip lesions,” affects the full bowel wall, and cannot be cured surgically.
Lifestyle factors like diet, hydration, stress control, and smoking habits also have different impacts on each disease. Advances in biologic therapies, targeted immunomodulators, and improved surgical techniques mean that with accurate diagnosis and individualized care, most people can achieve remission and protect their quality of life.
Understanding the nuances between these two conditions empowers patients, caregivers, and clinicians to make better treatment decisions and live well despite a chronic diagnosis.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Post You Might Like:
- 20 Daily Habits for a Happier Gut (Backed by Science)
- 15+ Powerful Fermented Foods for Gut Health (Complete Probiotic Guide)
- 8 Proven Ways Stress Wrecks Your Gut Health Fast
- 15 Warning Signs Your Gut Isn’t Absorbing Nutrients Properly (And What to Do About It)
- 12 Powerful Health Benefits of Coffee Backed by Science