
⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission — at no extra cost to you — if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
7 Proven Methods for Managing Chronic Low Back Pain Without Opioids
Chronic low back pain (CLBP) is more than just a nuisance, it’s a global health challenge that affects millions of people across all ages and walks of life. In fact, statistics show that nearly 1 in 6 adults worldwide suffer from persistent back pain lasting three months or more. This ongoing discomfort can sap your energy, reduce your mobility, disrupt sleep, and strain your emotional well-being. It can make everyday tasks, from standing and walking to working and socializing, difficult or even impossible.
For many years, opioids were commonly prescribed as a quick fix to dull the intense pain associated with chronic low back issues, while these medications can provide short-term relief, long-term reliance on opioids has revealed significant drawbacks from physical dependence and increased tolerance to a higher risk of serious side effects and accidental overdose. More importantly, research has shown that opioids often fail to deliver sustainable pain relief for chronic conditions like CLBP.
In today’s healthcare landscape, the focus is shifting toward safer, more holistic approaches that empower patients to manage pain effectively without the risks linked to opioid use. Advances in physical therapy, mind-body techniques, lifestyle adjustments, and alternative therapies have created a diverse toolkit for tackling chronic low back pain in a way that prioritizes long-term health and quality of life.
Whether you’re newly diagnosed, struggling to reduce your opioid use, or simply looking for natural ways to reclaim your comfort and mobility, this comprehensive guide will provide you with actionable strategies backed by science. You’ll learn how to combine medical treatments with lifestyle changes, exercises, mental health support, and ergonomic improvements all designed to reduce pain, restore function, and improve your overall well-being.
Managing chronic low back pain without opioids isn’t just about avoiding medications, it’s about taking control of your health and embracing a sustainable path to recovery and resilience.
Understanding Chronic Low Back Pain
Chronic low back pain is a complex condition that affects millions of people worldwide, often disrupting daily life and diminishing overall well-being. To effectively manage it, it’s crucial to understand what sets chronic pain apart from acute pain, as well as the common causes behind persistent discomfort. This foundational knowledge helps guide treatment choices and lifestyle modifications for lasting relief.
Acute vs. Chronic Low Back Pain
Low back pain generally falls into two categories based on duration and underlying causes:
Acute Low Back Pain:
Acute pain typically lasts less than six weeks. It often results from an identifiable injury or strain, such as lifting something heavy incorrectly, sudden twisting, or muscle overuse. The pain usually comes on suddenly and may be sharp or intense, because it’s often linked to tissue damage or inflammation, acute pain tends to improve as the body heals, with rest and conservative treatment.Chronic Low Back Pain:
When pain persists beyond 12 weeks, it is classified as chronic. Importantly, chronic low back pain may continue even after the initial injury has healed, indicating that other factors such as nerve sensitization, muscle weakness, or psychological influences, may be involved. Unlike acute pain, chronic pain can be constant or intermittent, ranging from dull and nagging to sharp or burning. It may also radiate from the lower back into the buttocks, thighs, or even down the legs, sometimes causing numbness or tingling.
Understanding this distinction is key because chronic pain requires a different approach to treatment, one that focuses on managing symptoms, improving function, and addressing underlying causes rather than just short-term relief.
Common Causes of Chronic Low Back Pain
Chronic low back pain is rarely caused by a single issue. Often, it results from a combination of factors that affect the spine, muscles, nerves, and surrounding tissues. Some of the most common causes include:
- Degenerative Disc Disease:
The intervertebral discs are cushion-like structures between the bones (vertebrae) of your spine. Over time, these discs can lose hydration and elasticity, becoming thinner and less effective at absorbing shock. This degeneration can cause pain, stiffness, and sometimes nerve irritation. - Osteoarthritis:
This “wear and tear” arthritis affects the facet joints in the spine, leading to cartilage breakdown, inflammation, and bone spurs. Osteoarthritis can cause localized back pain and stiffness, especially in older adults. - Spinal Stenosis:
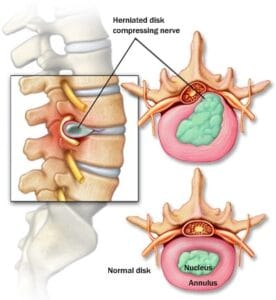
Spinal stenosis occurs when the spaces within your spine narrow, putting pressure on the spinal cord and nerves. This can cause pain, numbness, or weakness, often worsening with walking or standing for prolonged periods. - Herniated Discs:
Sometimes called slipped or ruptured discs, a herniated disc happens when the soft inner material of a disc pushes through its tougher exterior. This can compress nearby nerves, causing sharp pain, numbness, or weakness, especially if it affects the sciatic nerve.
through its tougher exterior. This can compress nearby nerves, causing sharp pain, numbness, or weakness, especially if it affects the sciatic nerve. - Muscle Imbalances and Weakness:
Weakness in the core muscles (abdomen, back, and hips) or tightness in muscles like the hamstrings and hip flexors can lead to poor spinal support and increased strain on the lower back. Over time, these imbalances contribute to chronic pain. - Poor Posture:
Spending long hours sitting or standing with improper alignment such as slouching or forward head posture places uneven pressure on the spine and muscles. This can lead to chronic strain and discomfort. - Inflammatory Conditions:
Certain autoimmune diseases, such as ankylosing spondylitis, cause inflammation of the spinal joints and ligaments. This can result in persistent back pain and stiffness that worsen over time. - Fibromyalgia:
A chronic condition characterized by widespread musculoskeletal pain, fatigue, and tenderness. Fibromyalgia can amplify pain sensations and is often accompanied by mood disorders and sleep disturbances. - Other Contributing Factors:
Psychological stress, obesity, smoking, and sedentary lifestyle can all contribute to chronic low back pain by increasing inflammation, reducing healing capacity, and worsening muscle function.
The Importance of Accurate Diagnosis
Because chronic low back pain can stem from diverse causes, proper diagnosis by a healthcare professional is essential. This may involve:
- Medical history and physical exam
- Imaging tests like X-rays, MRI, or CT scans
- Nerve conduction studies for neuropathic pain
- Blood tests for inflammatory markers
Understanding the specific cause helps tailor the most effective, non-opioid treatment plan for lasting relief.
Why Opioids Aren’t the First Choice
For many years, opioids were widely prescribed to manage moderate to severe chronic low back pain. However, extensive research and clinical experience have shown that opioids are not the ideal long-term solution for most patients with chronic low back pain. Here’s why:
Limited Effectiveness for Long-Term Pain Relief
Several high-quality studies have found that opioids do not provide superior pain relief compared to non-opioid medications or non-pharmacological treatments over the long term. While opioids may reduce pain temporarily, their benefits often diminish with extended use due to tolerance.
Risk of Physical Dependence and Addiction
Opioids are highly addictive substances. Over time, the body builds tolerance, meaning patients need higher doses to achieve the same level of pain relief. This can quickly lead to physical dependence and addiction, even when used as prescribed.
Opioid-Induced Hyperalgesia (Increased Pain Sensitivity)
Paradoxically, long-term opioid use may cause the nervous system to become more sensitive to pain, a phenomenon called opioid-induced hyperalgesia. This can worsen chronic pain and create a vicious cycle of increasing medication use.
Side Effects and Health Risks
Common opioid side effects include:
- Sedation and cognitive impairment, which can affect daily functioning.
- Constipation, which can be severe and chronic.
- Hormonal imbalances affecting mood, libido, and bone health.
- Respiratory depression in high doses, increasing overdose risk.
- Increased risk of falls and fractures, especially in older adults.
Societal Impact
The opioid epidemic has highlighted the dangers of overprescribing these medications, leading to a public health crisis with rising rates of addiction, overdose, and death.
In summary, opioids should generally be reserved for short-term use or carefully monitored cases, and safer alternatives should be prioritized for managing chronic low back pain.
The Core Principles of Non-Opioid Pain Management
Managing chronic low back pain effectively without opioids requires a multi-dimensional, holistic approach. This approach focuses on addressing the various factors contributing to pain and disability, rather than simply masking symptoms.
1. Addressing the Root Cause
Whenever possible, identify and treat the underlying cause of pain, such as muscle imbalances, joint dysfunction, or inflammation. This may involve:
- Corrective exercises to strengthen weak muscles and stretch tight ones.
- Postural corrections to reduce undue spinal stress.
- Treating inflammatory conditions or spinal abnormalities under medical supervision.
2. Improving Physical Function Through Exercise
Regular, controlled physical activity is one of the most effective ways to reduce chronic low back pain. Exercise:
- Strengthens core and back muscles to better support the spine.
- Increases flexibility to reduce stiffness.
- Enhances circulation, promoting tissue healing.
- Releases endorphins, the body’s natural painkillers.
Working with a physical therapist or trained professional can help tailor a safe and effective exercise program.
3. Reducing Inflammation
Chronic inflammation can worsen pain and tissue damage. Lifestyle and dietary changes, along with safe medications, can help reduce inflammation:
- Anti-inflammatory diets rich in omega-3 fatty acids, fruits, and vegetables.
- Avoidance of processed foods and excess sugar.
- Use of NSAIDs (short-term) or topical anti-inflammatory agents as recommended.
4. Supporting Mental Health
Chronic pain affects emotional well-being, and stress or anxiety can amplify pain perception. Integrative pain management includes:
- Cognitive Behavioral Therapy (CBT) to change pain-related thoughts.
- Mindfulness and relaxation techniques.
- Social support and counseling as needed.
5. Lifestyle Modifications to Prevent Flare-Ups
Small changes can make a big difference in pain control:
- Ergonomic improvements at work and home.
- Weight management to reduce spinal load.
- Smoking cessation to improve tissue oxygenation.
- Proper sleep hygiene to aid recovery.
Non-Opioid Medications and Topicals
While the goal is to minimize reliance on medications, certain non-opioid drugs and topical treatments can provide effective pain relief, especially when combined with other therapies.
Over-the-Counter (OTC) Options
- Acetaminophen (Paracetamol):
Commonly used for mild to moderate pain, acetaminophen works primarily in the brain to reduce the perception of pain. However, it does not address inflammation and is less effective for inflammatory causes of back pain. It is generally safe when used as directed but should be avoided in high doses due to potential liver toxicity. - Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):
Drugs like ibuprofen and naproxen reduce both pain and inflammation by blocking enzymes involved in the inflammatory process. NSAIDs are often more effective than acetaminophen for back pain with an inflammatory component. However, they should be used short-term due to potential side effects, including gastrointestinal irritation, kidney issues, and increased cardiovascular risk in some patients. - Topical NSAIDs:
These are gels, creams, or patches applied directly to the painful area. They provide localized relief with fewer systemic side effects compared to oral NSAIDs. Common options include diclofenac gel. Topical treatments can be especially useful for patients who cannot tolerate oral medications. - Capsaicin Cream:
Derived from chili peppers, capsaicin works by depleting substance P, a neurotransmitter involved in sending pain signals. Regular application can reduce nerve sensitivity and provide gradual pain relief. It can cause a burning sensation on application but is generally safe and non-addictive. - Menthol or Camphor Gels:
These produce cooling or warming sensations that distract the brain from pain signals (a process known as counterirritation). They provide temporary relief and are often used as adjuncts to other therapies.
Prescription Non-Opioid Medications
- Muscle Relaxants:
Prescribed for short-term relief of muscle spasms associated with back pain. Common drugs include cyclobenzaprine and methocarbamol. Side effects can include drowsiness and dizziness; therefore, they are usually limited to brief courses. - Antidepressants (SNRIs, TCAs):
Some antidepressants, like duloxetine (a serotonin-norepinephrine reuptake inhibitor) and amitriptyline (a tricyclic), have been shown to reduce certain types of chronic pain, including nerve-related pain. They work by modulating pain pathways in the brain and improving mood and sleep, which often helps reduce overall pain perception. - Anticonvulsants:
Medications such as gabapentin and pregabalin are used to treat neuropathic (nerve) pain. They calm nerve activity and can be effective in cases where nerve compression or irritation contributes to back pain symptoms.
Important Reminder: Always discuss your medications and pain management plan with a healthcare provider. Long-term use of any medication requires monitoring to avoid side effects, interactions, and diminishing effectiveness.
Physical Therapy and Exercise-Based Solutions
Why Movement Is Medicine
Contrary to popular belief, resting in bed or avoiding activity is often counterproductive for chronic low back pain, while acute injury may require short-term rest, prolonged inactivity can weaken muscles, reduce flexibility, and impair circulation, all factors that contribute to ongoing pain and stiffness.
Controlled and guided movement stimulates healing by strengthening the muscles that support the spine, improving joint mobility, and increasing blood flow to injured or inflamed tissues. Movement also triggers the release of endorphins, the body’s natural painkillers, which help reduce the perception of pain.
Types of Exercises That Help
Different types of exercises target various components of spinal health and pain management:
- Core Strengthening:
Strong core muscles (abdominals, obliques, and lower back muscles) act as a natural brace for the spine. Exercises like planks, bridges, and pelvic tilts improve stability and reduce the risk of re-injury. - Flexibility Training:
Tight muscles, especially in the hamstrings, hip flexors, and lower back, can pull on the spine and worsen pain. Gentle stretches, such as hamstring stretches and yoga poses like Cat-Cow, enhance flexibility and ease muscle tension. - Low-Impact Cardio:
Activities like walking, swimming, and cycling improve cardiovascular health without placing excessive strain on the back. Regular aerobic exercise helps reduce inflammation and promotes overall well-being. - Postural Training:
Poor posture contributes significantly to chronic back pain. Exercises like wall angels and seated alignment drills teach proper spinal alignment and help correct habitual slouching or forward head posture. - Stability Exercises:
Movements such as the bird-dog and side planks focus on improving balance and coordination of spinal stabilizers, which support proper movement mechanics.
Working with a Physical Therapist
A physical therapist (PT) is a valuable partner in managing chronic low back pain. A PT can:
- Assess Muscle Imbalances: Identify weak or tight muscles contributing to pain.
- Teach Safe Movement: Demonstrate proper lifting, bending, and posture techniques to avoid further injury.
- Provide Manual Therapy: Hands-on treatments like massage, mobilization, or myofascial release to reduce muscle tension and improve joint mobility.
- Create a Personalized Plan: Tailor exercises to your specific condition, limitations, and goals, ensuring safety and effectiveness.
Regular follow-ups with a PT help track progress and adjust the program as needed.
Mind-Body Approaches
1. Cognitive Behavioral Therapy (CBT)
CBT addresses the psychological component of chronic pain by helping individuals recognize and change negative thought patterns and behaviors related to their pain experience. It can reduce feelings of helplessness, anxiety, and depression that often accompany chronic pain and improve coping strategies.
2. Mindfulness and Meditation
Mindfulness practices cultivate a non-judgmental awareness of the present moment. Techniques such as body scans, deep breathing exercises, and guided imagery reduce stress, lower muscle tension, and decrease the brain’s amplification of pain signals.
3. Yoga and Tai Chi
These gentle mind-body exercises combine stretching, strength-building, and controlled breathing. Both have been shown in clinical studies to improve spinal flexibility, reduce pain intensity, enhance balance, and boost mental well-being.
Alternative and Complementary Therapies
- Acupuncture:
Insertion of fine needles at specific points may stimulate the release of endorphins and modulate nerve activity, providing pain relief for some patients. - Massage Therapy:
Targeted massage eases muscle tightness, improves circulation, and promotes relaxation, which can reduce pain and improve mobility. - Chiropractic Care:
Spinal manipulation and adjustments can restore proper joint function, reduce muscle tension, and alleviate pain in select cases, especially mechanical back pain. - Dry Needling:
This technique targets trigger points (knots) in muscles, releasing tension and reducing referred pain.
While alternative therapies can be effective adjuncts, it’s important to consult with healthcare providers to ensure safety and appropriateness.
Lifestyle and Ergonomic Adjustments
1. Workstation Setup
Poor ergonomics can worsen chronic back pain, especially for those working long hours at desks.
- Keep your computer screen at eye level to avoid neck strain.
- Use a chair with lumbar support to maintain natural spine curves.
- Take short standing or stretching breaks every 30-45 minutes to prevent stiffness and muscle fatigue.
2. Sleep Optimization
Quality sleep is essential for tissue repair and pain management.
- Use a medium-firm mattress that supports spinal alignment.
- Sleep on your side with a pillow between your knees to reduce spinal rotation and pressure.
- Avoid sleeping on your stomach, which can strain the neck and back.
3. Weight Management
Excess body weight increases mechanical load on the spine and joints, exacerbating pain. Even moderate weight loss through diet and exercise can significantly reduce symptoms.
4. Anti-Inflammatory Diet
Certain foods promote inflammation, while others help reduce it:
- Focus on fruits, vegetables, whole grains, lean proteins, and omega-3 fatty acids (found in fatty fish, flaxseeds, walnuts).
- Limit intake of processed foods, sugary drinks, refined carbs, and trans fats, which can worsen systemic inflammation.
Building a Sustainable Pain-Management Plan
1. Set Realistic Goals
Complete elimination of pain may not be immediately possible. Instead, aim for pain reduction and improved function, enabling you to participate in daily activities and enjoy life.
2. Track Your Triggers and Progress
Maintain a pain journal documenting:
- Activities that increase or decrease pain
- Dietary habits
- Sleep quality
- Stress levels
This data helps you and your healthcare team tailor treatment strategies.
3. Work with a Multidisciplinary Team
Chronic pain often requires care from various specialists, including:
- Physicians (primary care, pain specialists)
- Physical therapists
- Psychologists or counselors
- Nutritionists
- Occupational therapists
This collaborative approach addresses physical, emotional, and social aspects of pain.
When to Seek Immediate Medical Attention
While most chronic low back pain is manageable, certain symptoms require urgent medical evaluation:
- Sudden numbness, weakness, or loss of sensation in the legs or groin (possible nerve compression or spinal cord involvement)
- Loss of bladder or bowel control (sign of cauda equina syndrome, a medical emergency)
- Unexplained fever or weight loss (may indicate infection or malignancy)
- Severe trauma or injury (e.g., after a fall or accident)
If you experience any of these red-flag symptoms, seek emergency ca
Conclusion: Empowering Your Life Beyond Chronic Low Back Pain
Living with chronic low back pain can feel overwhelming, but it doesn’t have to define your life or limit your potential. Moving beyond reliance on opioids opens the door to safer, more sustainable strategies that address the root causes of your pain and support your overall well-being.
By embracing a balanced approach, combining targeted exercise, mindful mental health practices, thoughtful lifestyle changes, and evidence-based medical treatments, you can regain control over your body and your daily experiences. Each positive step, no matter how small, builds resilience, reduces discomfort, and enhances your mobility and independence.
Remember, managing chronic pain is a journey, not a quick fix. With patience, support, and determination, lasting relief is within reach. Your body is capable of healing, and your mind is powerful enough to transform how you experience pain. Together, these strengths can help you reclaim a vibrant, fulfilling life, free from the shadow of chronic low back pain.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Blog Post You Might Like:
- Does Physical Therapy Help with Neck Pain? 7 Powerful Research Backed Facts
- 7 Powerful Supplements for Diabetic Nerve Pain Relief (Backed by Science)
- Can a Chiropractor Help with Nerve Pain in the Feet? The Truth Explained
- 7 Alarming Signs of Vitamin D Deficiency Fatigue and Joint Pain
- 10 Effective Foot Exercises for Neuropathy to Improve Circulation and Relieve Nerve Pain
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being

 through its tougher exterior. This can compress nearby nerves, causing sharp pain, numbness, or weakness, especially if it affects the sciatic nerve.
through its tougher exterior. This can compress nearby nerves, causing sharp pain, numbness, or weakness, especially if it affects the sciatic nerve.
