⚠️ Affiliate Disclaimer: This post may contain affiliate links, which means I may earn a small commission — at no extra cost to you — if you make a purchase through one of these links. I only recommend products or services I genuinely trust and believe can provide value. Thank you for supporting My Medical Muse!
How to Interpret Hemoglobin A1c Levels: 10 Proven Tips for Accuracy
When you look at a blood test report, few numbers carry as much weight as hemoglobin A1c (HbA1c). Doctors use it to diagnose diabetes, track long-term blood sugar control, and estimate the risk of complications affecting the nerves, kidneys, eyes, and heart. Yet despite how commonly it is ordered, HbA1c is also one of the most misunderstood lab values.
If you have been told you are diabetic, prediabetic, or “borderline,” your HbA1c often becomes the headline number that defines your health but interpreting it correctly takes more than knowing whether it falls above or below a cutoff. HbA1c is not a simple good-versus-bad score. It is an average influenced by biology, lifestyle, and even factors unrelated to blood sugar itself.
Age, ethnicity, red blood cell lifespan, nutrient deficiencies, and other glucose measurements all shape what your HbA1c actually represents. Two people can have the same HbA1c and very different blood sugar patterns and risks. That is why context matters as much as the number.
This guide breaks HbA1c down clearly and practically. You will learn how the test works, what each range truly means, when results can be misleading, and how to improve your numbers safely using evidence-based strategies rather than guesswork.
By the end, you will be able to look at your HbA1c result and understand what it is really telling you about your long-term blood sugar health.
What is Hemoglobin A1c?
The science behind the test
Your blood contains red blood cells packed with hemoglobin, the protein that carries oxygen. When you have sugar (glucose) in your blood, some of it naturally attaches to hemoglobin in a process called glycation. The more sugar in your blood, the more hemoglobin gets “glycated” because red blood cells live for about 90-120 days, HbA1c gives an average of your blood sugar over the last 2-3 months.
Why it’s better than a single glucose reading
- Fasting glucose only reflects your sugar level at the moment of testing.
- HbA1c smooths out the ups and downs, showing a long-term trend.
- This makes it a better predictor of complications risk like nerve damage, kidney disease, and eye problems.
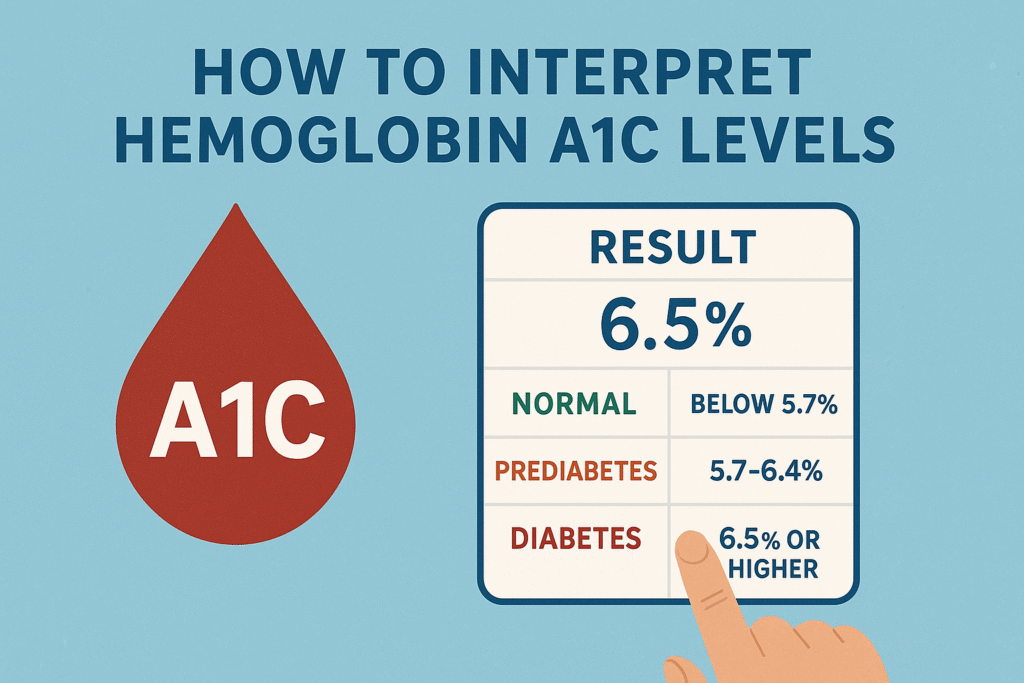
Standard HbA1c Ranges and What They Mean
| HbA1c % | Category | Average Glucose (mg/dL) | Average Glucose (mmol/L) | What it means for your health |
| Below 5.7% | Normal | <117 | <6.5 | Healthy blood sugar control, low diabetes risk. |
| 5.7% – 6.4% | Prediabetes | 117–137 | 6.5-7.6 | Higher than normal; increased risk of developing type 2 diabetes and heart disease. |
| 6.5% – 7.0% | Diabetes (well-controlled) | 137–154 | 7.6-8.6 | Meets diabetes criteria; at target for most patients. |
| 7.1% – 8.0% | Diabetes (needs improvement) | 155–183 | 8.7-10.1 | Above recommended target for many; higher risk of complications. |
| Above 8.0% | Poorly controlled diabetes | >183 | >10.1 | Significantly increased risk of complications; treatment review needed. |
How HbA1c Relates to Your Average Blood Sugar
Your HbA1c number isn’t just a random percentage, it can actually be translated into an average blood sugar level, which is easier for most people to picture. Doctors often use something called Estimated Average Glucose (eAG) for this.
Think of it like this:
- HbA1c: a report card of your blood sugar over the last 3 months.
- eAG: what that “grade” means in day-to-day numbers, like the readings you’d see on a glucose meter.
Here’s the formula doctors use:
eAG (mg/dL): (28.7 × HbA1c) – 46.7
Example:
Let’s say your HbA1c is 7.5%.
- First, multiply: 28.7 × 7.5 = 215.25
- Then subtract: 215.25 – 46.7 = 168.55 mg/dL
- In mmol/L (used in some countries), that’s about 9.35 mmol/L.
What this means in real life:
If your HbA1c is 7.5%, your blood sugar has averaged roughly 169 mg/dL every day over the past three months including after meals, during sleep, and in between snacks.
It’s like taking every single blood sugar reading you would’ve gotten for 90 days, adding them all up, and finding the average. This gives you a clearer picture of your overall control, even if you don’t test your blood sugar often.
Factors That Can Skew HbA1c Results
HbA1c is a great tool for tracking long-term blood sugar, but it’s not perfect. Sometimes the number you get doesn’t match what’s really happening in your body.
There are two main types of errors: false highs (when HbA1c looks worse than it is) and false lows (when it looks better than it is).
False Highs: When HbA1c Shows a Higher Number Than Reality
These situations can make it seem like your blood sugar has been higher than it actually has:
- Iron deficiency anemia When your body doesn’t have enough iron, your red blood cells live longer than usual. The longer they live, the more sugar they collect, which makes your HbA1c appear higher.
- Vitamin B12 or folate deficiency, These vitamins are needed to make healthy red blood cells without them, your cells live longer, again giving sugar more time to stick to them.
- Chronic kidney disease Waste products in the blood (uremic toxins) can change how hemoglobin behaves, leading to misleading HbA1c results.
- Heavy alcohol use: Alcohol can change how your body processes hemoglobin, making it appear more “sugar-coated” than it really is.
False Lows: When HbA1c Shows a Lower Number Than Reality
These situations can make it seem like your blood sugar is better controlled than it actually is:
- Recent blood loss or transfusion: New blood cells from your own body or from a transfusion have little or no sugar coating, which pulls the average down.
- Hemolytic anemia: This condition makes red blood cells break down faster than normal, so they don’t live long enough to collect much sugar.
- Recent treatment for anemia: If you just started iron, B12, or folate supplements, your body quickly produces lots of fresh red cells with low sugar, lowering your HbA1c.
- High doses of vitamin C or E: These antioxidants can interfere with some lab methods, giving you an artificially low reading.
If your HbA1c doesn’t seem to match your home glucose readings, it could be due to one of these factors, not just your blood sugar control. In those cases, your doctor may use other tests, like fructosamine, to get a clearer picture.
Ethnic Variations: Why Your Background Might Affect HbA1c
Research shows that some people naturally have slightly higher HbA1c levels even if their actual blood sugar is the same as someone from another ethnic group.
- Who this affects most: Studies have found this pattern more often in African, Hispanic/Latino, and some Asian populations.
- Why this happens: It’s believed to be linked to genetic differences in how hemoglobin is structured or how long red blood cells live in the body.
- What this means for you:
- A slightly higher HbA1c doesn’t automatically mean you’re doing poorly with your blood sugar control.
- Your doctor might put more weight on daily glucose checks, post-meal readings, or CGM data when making decisions.
- A slightly higher HbA1c doesn’t automatically mean you’re doing poorly with your blood sugar control.
Think of it like two cars that both drive the same speed, but one car’s speedometer reads a little higher. The actual speed hasn’t changed, it’s just the measurement tool that’s a bit different.
Putting HbA1c Into Context
HbA1c is a valuable number, but it should never be the only thing you look at when judging your blood sugar health. Here’s why:
Other Tests That Complement HbA1c
Relying on HbA1c alone is like reading just the last page of a book, you miss important details about the story these other tests fill in the gaps:
Fasting Blood Glucose
- Measures sugar levels after 8-12 hours without food (often done in the morning before breakfast).
- Shows how well your body manages sugar overnight without the influence of meals. Example, if your HbA1c looks okay but your fasting sugar is high, it could point to dawn phenomenon (early morning sugar spike).
- Measures sugar levels after 8-12 hours without food (often done in the morning before breakfast).
Postprandial Glucose (After-Meal Reading)
- Taken 1-2 hours after eating.
- Reveals how your body handles sugar from food.
- Example: Two people could both have an HbA1c of 6.5%, but one might have big after-meal spikes that increase heart risk and this wouldn’t show in HbA1c alone.
- Taken 1-2 hours after eating.
Continuous Glucose Monitoring (CGM):
- A small sensor tracks your sugar levels all day and night.
- Shows patterns, swings, and how foods, exercise, or stress affect you in real time.
- Especially useful if you want to avoid surprises like hidden highs or nighttime lows.
- A small sensor tracks your sugar levels all day and night.
Individualized Targets- One Size Doesn’t Fit All
The “perfect” HbA1c goal depends on your age, health status, and personal circumstances.
Here’s a practical breakdown:
- Healthy Adults:
Aim for 6.5-7.0%. This keeps blood sugar close to normal while minimizing the risk of low sugar episodes. - Older Adults or Those with Other Health Conditions:
A goal of 7.5-8.0% can be safer, especially if you’re at higher risk of dangerous lows.
Example: An 80-year-old with heart issues might benefit from a gentler target to avoid fainting from low blood sugar. - Pregnant Women:
Often advised to stay below 6.0% (sometimes even 5.7%) because tight control helps prevent complications for the baby.
Example: High sugars during pregnancy can increase the baby’s risk of being born very large or having low sugar after birth.
Your HbA1c is important, but it’s just one piece of your health puzzle. It works best in combination with other tests and personalized goals set with your healthcare provider.
How Often Should You Test HbA1c?
- No diabetes, at risk: Every 12 months
- Prediabetes: Every 6-12 months.
- Diabetes, stable: Every 6 months.
- Diabetes, unstable or treatment changes: Every 3 months
Evidence-Based Strategies to Improve HbA1c
Nutrition:
One of the most effective ways to improve HbA1c is by making intentional changes to your eating habits. Aim to eat balanced meals that combine carbohydrates with sources of protein and healthy fats, this slows digestion helps keep blood sugar from spiking sharply. Increasing your intake of dietary fiber is another game changer. Foods like vegetables, legumes, and whole grains help regulate blood sugar by slowing glucose absorption into the bloodstream.
On the flip side, limiting sugary drinks, white bread, and pastries is essential because these foods are digested quickly, leading to rapid blood sugar rises. Meal timing also matters more than many people realize, spreading your carbohydrate intake evenly throughout the day and avoiding large, late-night carb-heavy meals can prevent overnight and early-morning spikes.
Exercise:
Physical activity is a powerful tool for improving insulin sensitivity and lowering HbA1c. Aiming for at least 150 minutes of moderate aerobic activity per week, such as brisk walking, cycling, or swimming, it can make a significant difference. Including resistance training at least twice a week, like weight lifting or bodyweight exercises, helps build muscle, which in turn improves your body’s ability to use glucose effectively.
Even light movement after meals, such as a 10-15 minute walk, can help lower post-meal blood sugar spikes by encouraging your muscles to use circulating glucose right away.
Weight Management
For individuals who are overweight, even modest weight loss can lead to noticeable improvements in HbA1c. Research shows that losing just 5-7% of body weight can enhance insulin sensitivity and reduce average blood sugar levels. This doesn’t mean extreme dieting, it can be achieved through gradual, sustainable changes to eating habits and regular physical activity. The goal is not perfection but consistent, realistic progress.
Medication
When lifestyle changes alone aren’t enough, medications play a critical role in controlling blood sugar. It’s important to take them exactly as prescribed and to communicate with your healthcare provider if you experience any side effects. In some cases, newer diabetes medications such as GLP-1 receptor agonists or SGLT2 inhibitors not only help lower HbA1c but also offer added heart and kidney protection. The right medication plan should be individualized based on your health profile, needs, and lifestyle.
Sleep and Stress
Many people overlook the impact of sleep and stress on blood sugar, but both are closely linked to HbA1c. Poor sleep and chronic stress raise cortisol levels, a hormone that can cause blood sugar to rise.
Over time, this makes it harder to keep HbA1c in the target range. Strive for 7-8 hours of quality sleep each night by maintaining a consistent bedtime and creating a calming pre-sleep routine. Stress management is equally important, whether it’s through meditation, deep breathing exercises, gentle yoga, or simply taking breaks during a busy day. These small but consistent practices can help keep both your mind and blood sugar in balance.
Alternative or Supportive Markers
- Fructosamine: Shows 2-3 week glucose trends (useful if HbA1c unreliable).
- Glycated albumin: Short-term average glucose marker.
- CGM “Time in Range”: Tracks % of time glucose stays in healthy range.
Avoiding Common Misinterpretations
A healthy HbA1c is a great sign, but it’s not the full picture, many people misinterpret what the number truly means and make decisions that could harm their long-term health. Here are three of the most common misconceptions:
“My HbA1c is fine, so I can eat anything.”
- Even with a good HbA1c, your daily blood sugar patterns might include large spikes after meals. These spikes can still damage blood vessels, nerves, and organs over time. HbA1c is an average, so it doesn’t reveal short-term fluctuations that contribute to complications. Balanced eating and glucose monitoring are still essential.
“A sudden drop is always good.”
- While lowering HbA1c is beneficial, doing so too quickly, especially for those with long-standing high blood sugar can cause unexpected problems. Rapid improvement can sometimes lead to temporary vision changes or worsen nerve pain. Healthcare professionals usually aim for gradual, controlled improvement to reduce these risks.
“It’s the same for everyone.”
- HbA1c results can be influenced by more than just blood sugar. Ethnicity, red blood cell lifespan, and lab testing variations can all affect the reading. For instance, african, hispanic, and some asian populations may naturally have slightly higher HbA1c levels at the same glucose concentrations. This is why your result should be interpreted alongside other tests like fasting glucose, post-meal readings, or continuous glucose monitoring.
In short, HbA1c is a valuable tool but it’s not a stand-alone measure of diabetes control. Context matters, and results should always be viewed as part of the bigger health picture.
Key Takeaways
- Normal: <5.7%
- Prediabetes: 5.7-6.4%
- Diabetes: ≥6.5%
Always interpret in context, other labs, lifestyle, and health conditions matter. Work with a healthcare provider to set personalized goals.
Bottom Line:
Your HbA1c is more than just a number, it’s a snapshot of your long-term blood sugar trends. But numbers don’t tell the whole story, the real power comes from knowing why your result looks the way it does and using that knowledge to make smart, consistent choices. Pair your HbA1c with daily habits that support steady blood sugar, and you’re not just managing diabetes, you’re taking control of your future health.
👩⚕️ Need Personalized Health Advice?
Get expert guidance tailored to your unique health concerns through MuseCare Consult. Our licensed doctors are here to help you understand your symptoms, medications, and lab results—confidentially and affordably.
👉 Book a MuseCare Consult NowRelated Blog Post You Might Like:
- Can Intermittent Fasting Help Type 2 Diabetes? 9 Powerful Facts
- Diabetes Mellitus: 10 Essential Insights on Causes, Types, Symptoms, Complications, and Modern Management
- Difference Between Type 1 and Type 2 Diabetes: 17 Critical Biological Differences Explained
- Unexplained Weight Loss or Gain in Diabetes: 11 Shocking Reasons It Happens
- 10 Critical Insights Into Blurred Vision in Diabetes: Temporary Changes vs Dangerous Damage
- 7 Alarming Ways Heart Disease and Diabetes Are Secretly Linked
Dr. Ijasusi Bamidele, MBBS (Binzhou Medical University, China), is a medical doctor with 5 years of clinical experience and founder of MyMedicalMuse.com, a subsidiary of Delimann Limited. As a health content writer for audiences in the USA, Canada, and Europe, Dr. Ijasusi helps readers understand complex health conditions, recognize why they have certain symptoms, and apply practical lifestyle modifications to improve well-being


